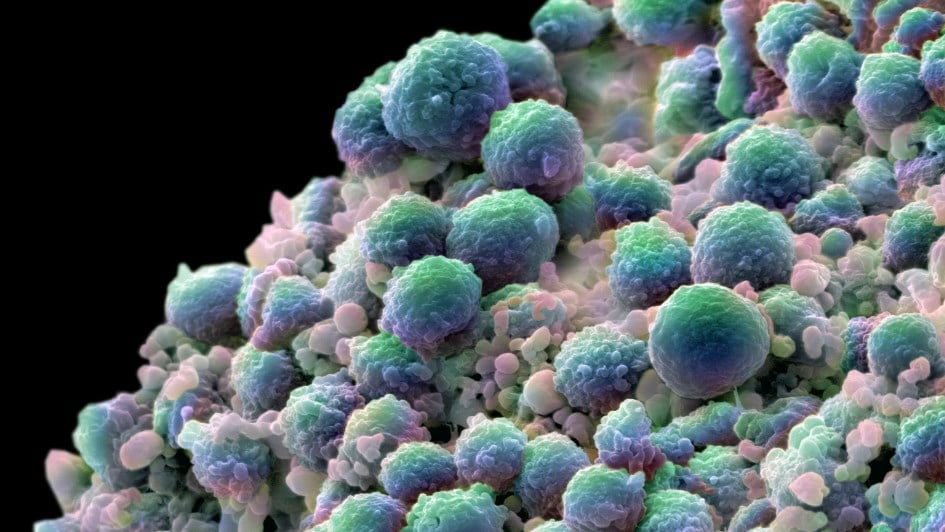
Image: Prostate cancer cells.
Researchers have found a way to predict which patients are likely to respond to radium-223, a standard treatment for advanced prostate cancer that has spread to the bones.
By using an imaging technique called an 18F-sodium fluoride (18F-NaF) PET scan, clinicians could ensure that they are only using this treatment for people who have a good chance of benefitting from it.
Until now, clinicians have had to use the same treatment approach for all patients with this form of cancer, even though it does not always produce results. Being able to better target treatment to the individual could extend survival and improve quality of life.
Trialling two different approaches
In the study, researchers analysed 133 lesions in 36 patients with castration-resistant prostate cancer that had spread only to the bones. They performed whole-body MRI with diffusion-weighted imaging at the start of the study and every eight weeks throughout, using this proven technique to monitor the change in apparent diffusion coefficient, or ADC, which serves to indicate the movement of water within a tissue.
The less the water can move, meaning a low ADC value, the higher the cellular density of the tumour – a hallmark of a more aggressive cancer. Based on data from other research, the team considered an increase in ADC of 30 per cent or more as indicative of a real treatment benefit.
Alongside this known method, the researchers carried out PET scans with 18F-NaF and 18F-choline. They found that the uptake of 18F-NaF by metastases at baseline was significantly higher in those that went on to produce an increase in ADC of 30 per cent or more. This means that a higher uptake of 18F-NaF prior to treatment correlates with a better response to treatment. However, there was no association between treatment response and 18F-choline uptake.
The team chose to trial this technique on the basis that radium-223, an internal form of radiotherapy, tends to be most effective in areas where the bone turnover rate is high. Cancer cells in bone metastases raise the turnover rate by releasing proteins that interfere with healthy bone cells, overactivating the cells that break down bone. As 18F-NaF is very similar in structure to calcium, which is key for bone development and metabolism, the uptake of the marker is significantly higher in bones with a high turnover rate.
A PET scan can reveal the areas with the highest uptake of 18F-NaF, thereby showing where radium-223 is most likely to work.
The study involved researchers from The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, and it was published in the journal European Radiology. The work was funded by the University of Basel, Bayer, the Cancer Research UK Convergence Science Centre at the ICR, and the National Institute for Health and Care Research (NIHR) Biomedical Research Centre and the Clinical Research Facilities at The Royal Marsden.
The difficulty of monitoring treatment response adds to the challenge of treating bone metastases
Advanced prostate cancer often spreads to the bones, causing bone metastases. Unlike with tumours or malignant lymph nodes, which shrink if treatment is effective, it is not possible to assess response to treatment by observing bone metastases. Instead, clinicians have to determine the effectiveness of treatment by considering survival and quality of life.
A different Royal Marsden and ICR-led study recently demonstrated that it was possible to use diffusion-weighted MRI, an imaging technique that studies the movement of water molecules in a tissue, to assess response to radium-223.
In addition, the researchers showed that some patients seemed to benefit much more than others from radium-223 treatment. Furthermore, different metastases within the same patient did not all respond in the same way. The most surprising finding, though, was that in some patients, new bone metastases developed during treatment.
The study was funded by Bayer, the Cancer Research UK Convergence Science Centre at the ICR, and the NIHR Biomedical Research Centre at The Royal Marsden and the ICR. It was published in the journal JNCI Cancer Spectrum.
First author Professor Chris Parker, Consultant in Clinical Oncology and Prostate Cancer at The Royal Marsden and Professor of Prostate Oncology at the ICR, said:
“This is exciting from a clinical point of view. Radium-223 has been used globally for more than a decade, but we’ve never before had a good way to assess response. We have tended to assume that all patients benefit to a similar extent, but we now know that’s not the case. What’s next is to try to predict response so that we can identify who might respond well to treatment.”
Bringing together recent findings
In combination, these two pieces of research represent a significant step forwards in the treatment of advanced prostate cancer that has spread to the bones.
Clinicians with access to the required technology could, subject to approval, use 18F-NaF PET to determine which patients are likely to respond to radium-223. They could then use diffusion-weighted MRI to monitor their response to treatment and confirm that it is proving effective.
This could potentially benefit all patients, as those who 18F-NaF PET did not identify as candidates for radium-223 treatment could receive an alternative treatment that may work better for them.
Senior author of the European Radiology paper Professor Dow-Mu Koh, who is Consultant Radiologist in Functional Imaging at The Royal Marsden and Professor in Functional Cancer Imaging at the ICR, said:
“This trial was innovative in its ambition to look at advanced imaging techniques side by side to see which can best inform decision-making around disease management. Our findings demonstrate how sensitive imaging is and how it can be used for targeted treatments. We hope that the study will be part of a paradigm shift in terms of how we monitor treatment for people with this form of cancer.”
Dr Matthew Blackledge, leader of the Computational Imaging Group at the ICR, brought his imaging expertise to this study. He said:
“We are pleased to confirm the predictive power of using PET, which might allow clinicians to stratify patients at an earlier timepoint. Alongside this, thanks to other work at the ICR, we can now use quantitative MRI to assess whether individual tumours are responding rather than the patient as a whole. This is particularly important when using radium-223. We hope that our findings will translate to wider clinical use so that as many patients as possible can benefit.”