Help every man with prostate cancer
Give the gift of research to help every man with prostate cancer live longer, healthier lives.
Tony McHale (pictured above) discovered he had an alteration in the BRCA2 gene at the age of 61, putting him at a much higher risk of developing prostate cancer. Shortly after, Tony joined the IMPACT study at the ICR, which investigated whether regular screening would lead to earlier diagnosis of aggressive forms of the disease. Around 18 months later, the screening revealed Tony had prostate cancer.
"Being involved in the IMPACT study saved my life. If I hadn't taken part, I'd never have known I had prostate cancer. As far as I was aware, I didn't have any symptoms – and the sooner the disease is detected and treated, the better the chances are of survival." – Tony
Godfrey's prostate cancer story
DJ and music promoter, Godfrey Fletcher, found out he had prostate cancer in 2015 at the age of 47, shortly after his father had also been diagnosed.
"I was so lucky that my cancer was picked up at a very early stage. I was young and fit, with no symptoms. A year after my treatment finished, I was told it had been successful. My dad wasn't so fortunate. He was diagnosed with advanced prostate cancer and passed away at 80. His experience, and mine, showed me the importance of early diagnosis."
Why we need more research into prostate cancer
We're proud of the research advances we've made over the last 20 years. Our scientists discovered the drug abiraterone; identified genetic variants that influence risk of developing the disease; and pioneered new, more precise forms of radiotherapy. But despite our research advances, some prostate cancers remain difficult to treat. This includes those diagnosed at a later stage and those more aggressive tumours, which can spread quickly and evolve to resist treatment.
That's why we urgently need better ways to detect prostate cancer earlier, predict drug resistance, and develop smarter, more personalised treatments. Your gift will help our world-leading researchers unravel the complexity of prostate cancer, to give men precise and personalised care with the right treatments at the right time, to live longer and healthier lives.
Professor Eeles's goal is to develop new tests that could be used in prostate cancer screening, helping to identify men at a higher risk. Her team showed that a simple saliva test, carried out at home, was more accurate at identifying future risk of prostate cancer for some men than the current standard blood test.
Building on this success, they recently launched a major new study to find out whether an improved version of this test – now suitable for more diverse groups, including Black men and younger men – can help detect more cancers earlier in men at higher risk.
Tackling drug resistance
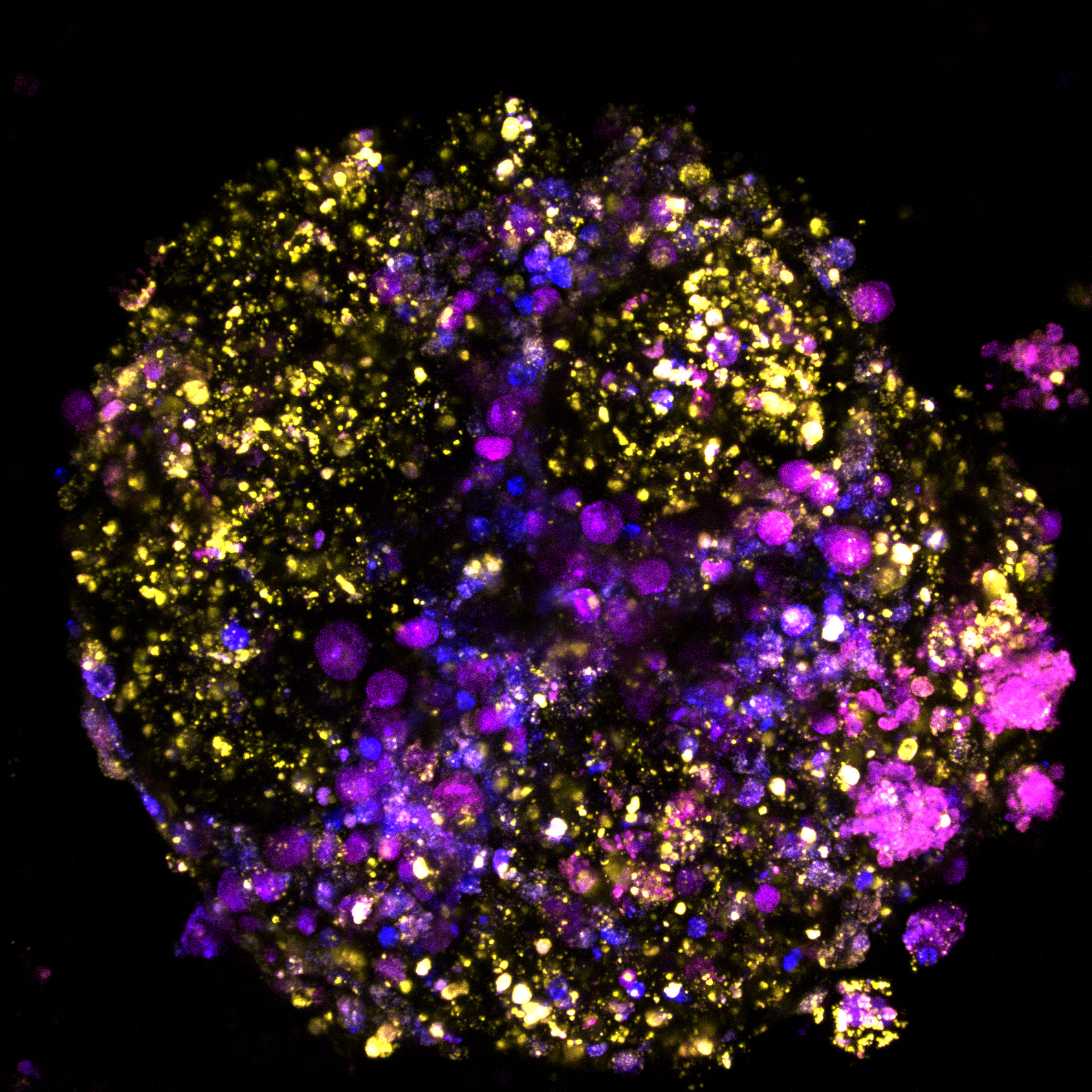
Our research underpinned the development of olaparib, a drug that revolutionised treatment for people with BRCA-related cancers. In a recent study, Professor Johann de Bono's team showed that changes which can be spotted with a simple blood test can reveal how long a prostate cancer patient will respond to olaparib.
The ability to predict when – and how – patients will stop responding to olaparib could help doctors personalise treatment, and in the future, guide the development of new drugs to outsmart resistance – keeping us one step ahead of prostate cancer.

Creating smarter, kinder treatments for every man
Our scientists are at the forefront of precision cancer medicine – developing more effective treatments with fewer side effects.
Laboratory studies co-led by Dr Adam Sharp and Professor Johann de Bono showed that NXP800 – a new drug which targets a ‘master switch’ that cancer cells hijack to support their growth – slowed prostate cancer cell growth. This innovative drug could potentially also benefit men with advanced prostate cancer that has stopped responding to standard hormone therapy.
A study co-led by Professor Emma Hall has found that men with intermediate-risk, localised prostate cancer can be treated just as effectively with five sessions of higher-dose radiation therapy as with several weeks of standard treatment. Using stereotactic body radiotherapy (SBRT), which targets tumours with pinpoint accuracy, patients can receive a highly effective treatment with far fewer hospital visits.
A study co-led by Professor Nick James has shown that a new artificial intelligence (AI) test can select which men with high-risk prostate cancer that has not spread will require the life-extending drug abiraterone. In the STAMPEDE trial, the team found that three out of four men could be spared unnecessary treatment, making the drug – discovered by our scientists – more affordable for the NHS.
Your gift can help every man with prostate cancer live longer, healthier lives
Help someone's dad, grandad, brother, uncle, partner, or friend survive prostate cancer. Your support will help fund life-saving research – so that every man can spend more precious time with their loved ones.




.tmb-hbmobile.png?Culture=en&sfvrsn=b703e5b1_1)