Timeline: How the ICR has led the way in prostate cancer research
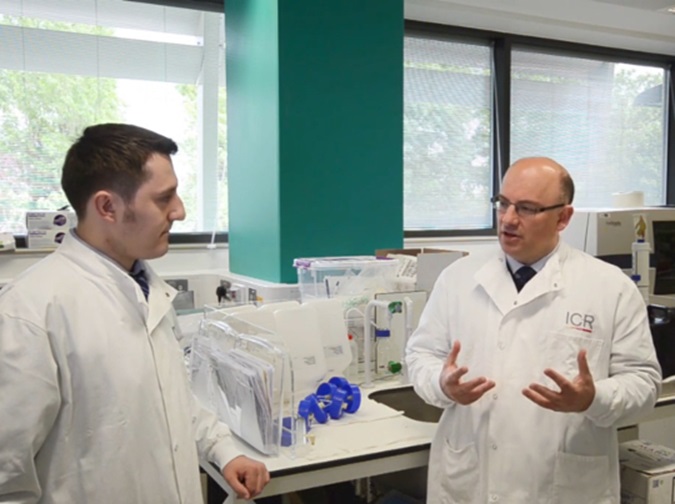
From ground-breaking clinical trials to innovative discoveries, The Institute of Cancer Research, London, has been pioneering new screening tools and treatments for prostate cancer for decades.
One of our biggest success stories is that of abiraterone, a drug that has now become a standard of care for advanced prostate cancer, benefiting hundreds of thousands of men worldwide.
Our scientists have been at the forefront of many other research advances that are making a difference to the lives of prostate cancer patients, including identifying genetic variants that influence risk of developing the disease and pioneering more precise forms of radiotherapy.
.tmb-ctadt.jpg?Culture=en&sfvrsn=d0c8e3d2_1)
1990s
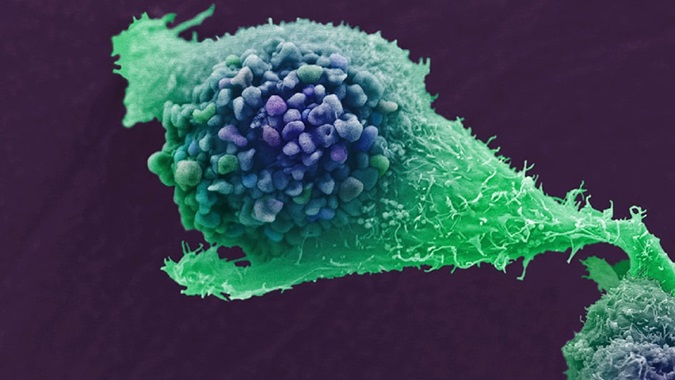
- In the 1990s, scientists at The Institute of Cancer Research (ICR), looking for ways to turn off the production of male sex hormones that drive prostate cancer, discovered abiraterone acetate. This became the first treatment shown to be effective in men with advanced prostate cancer.
- In 1993, the ICR and The Royal Marsden NHS Foundation Trust launched the UK Genetic Prostate Cancer Study (UKGPCS) – the largest prostate cancer study of its kind – to find genetic changes associated with prostate cancer risk. The final treatment updates will be collected by the end of 2027.
2000s
- In 2000, a team of scientists based at the ICR and The Royal Marsden became the first internationally to treat prostate cancer patients with a new, more precise form of radiotherapy, called intensity-modulated radiotherapy (IMRT). IMRT had been developed concurrently by several individuals in 1989, including Professor Steve Webb at the ICR.
- In 2004, the ICR’s groundbreaking discovery of the overactive E2F3 gene in prostate cancer tumours allowed doctors, for the first time, to predict the aggressiveness of the cancer.
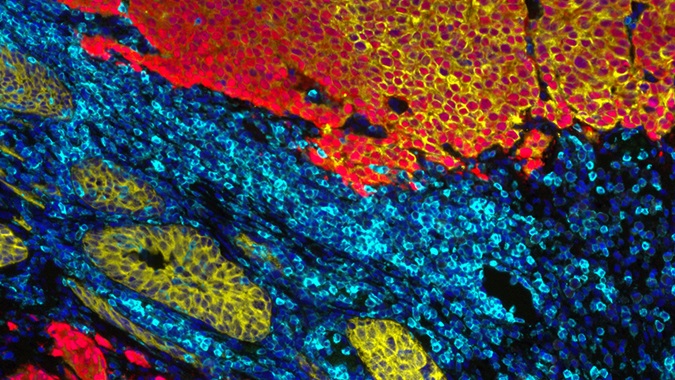
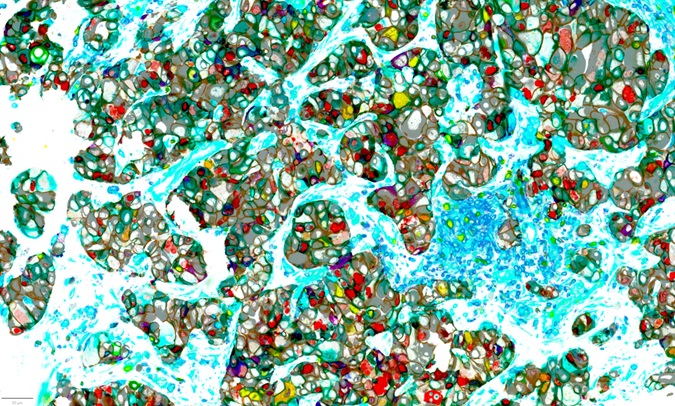
- In 2005, ICR researchers developed the Checkerboard Tissue Microarray (TMA) Method – a simple and highly reliable technique for analysing needle biopsy samples. The method looks for multiple markers of various genes associated with prostate cancer, including the E2F3 gene.
.tmb-ctadt.jpg?Culture=en&sfvrsn=b5833618_1)
- In 2007, scientists at the ICR and the Wolfson Institute of Preventive Medicine discovered a genetic change that identifies a particularly aggressive form of prostate cancer. The study found that the 6.6 per cent of prostate cancer patients with this 2+Edel marker have a 25 per cent survival rate after eight years, compared with 90 per cent for patients with no alterations in this region of DNA.
- In 2008, a phase I clinical trial led by Professor Johann de Bono revealed that abiraterone could treat up to 80 per cent of patients with aggressive and drug-resistant prostate cancer.
2010s
- In 2012, phase III trial data showed that abiraterone doubled the time before tumour progression could be detected by a scan in men who had no or mild symptoms and had not received chemotherapy. The benefits were so striking that the trial, led by the ICR and The Royal Marsden, was stopped early so that all participants could receive abiraterone.
- In 2012, the US Food and Drug Administration (FDA) approved abiraterone, in combination with the steroid prednisone, for use in patients before chemotherapy.
- In 2012, abiraterone was recommended by the National Institute for Health and Care Excellence (NICE) for use on the NHS in England, Wales and Northern Ireland to treat prostate cancer that has stopped responding to standard hormone therapies and docetaxel chemotherapy.
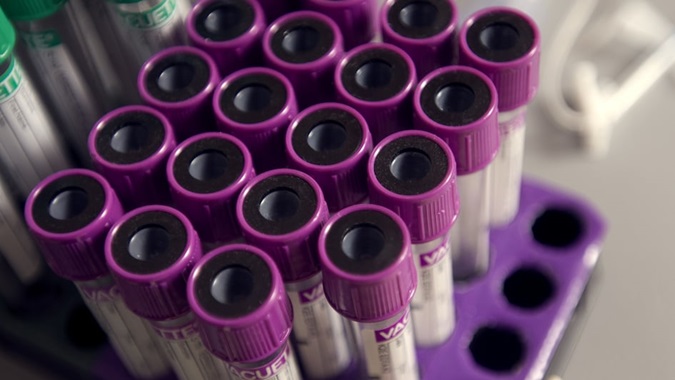
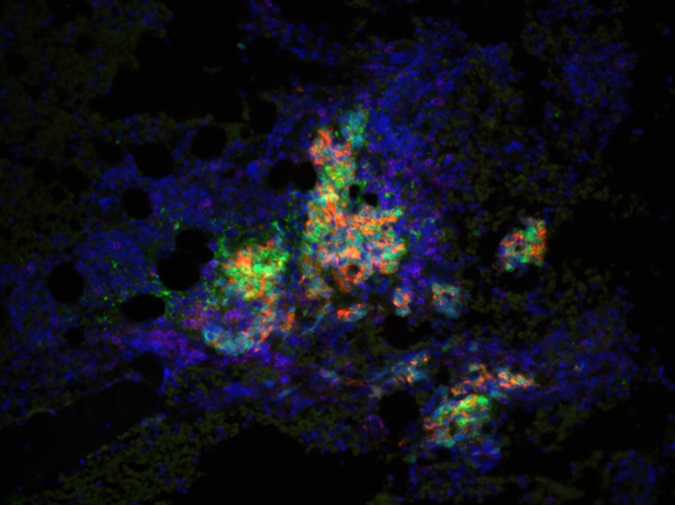
- In 2012, an ICR-led team designed a blood test that reads genetic changes like a barcode. By reading the pattern of genes switched on and off in blood samples, the researchers could accurately detect which advanced prostate cancer patients had the worst chance of survival.
- In 2013, the ICR conducted an analysis of the past decade’s data from 442 UK patients across 32 clinical trials and two extended access drug programmes at The Royal Marsden. This revealed that men with incurable prostate cancer were living more than twice as long as a decade earlier, thanks to new drugs such as abiraterone, enzalutamide and docetaxel.
- In 2013, research from the ICR and The Royal Marsden, led by Professor Chris Parker, showed that active surveillance – monitoring for disease progression rather than providing treatment – is a safe and effective option for men with low-risk localised prostate cancer.
- In 2014, ICR’s phase III RT01 trial, led by Professor David Dearnaley, showed that higher-dose radiotherapy better controls localised prostate cancer and reduces the need for hormone therapy. Based on these findings, NICE updated its guidance.

- In 2015, ICR researchers collaborated with eight academic clinical trial centres around the world to create a comprehensive map of the genetic mutations within lethal prostate cancers that have spread around the body.
- In 2015, an ICR-led clinical trial was the first to show the benefits of precision medicine in prostate cancer. The findings demonstrated that the targeted drug olaparib benefited prostate cancer patients with mutations in their DNA repair genes.
- In 2016, the results from a the 14-year CHHiP clinical trial led by the ICR and The Royal Marsden, and managed by the ICR Clinical Trials and Statistics Unit, revealed that delivering fewer, higher doses of radiation (20 dose schedules compared with 37) did not impact survival or quality of life and could save the NHS tens of millions of pounds per year.
- In 2016, radium-223, a radioactive drug, became routinely available on the NHS in England and Wales for men with advanced prostate cancer and bone metastases after ICR-led trials showed that it can extend survival and improve the quality of life for these patients.
- In 2017, long-term follow-up results from a trial led by the ICR and The Royal Marsden confirmed that IMRT was a safe treatment, producing strong survival rates with low toxicity. The trial, one of the first ever on IMRT, transformed treatment for many people with previously incurable prostate cancer.
- In 2017, researchers at the ICR developed two blood tests to enable personalised treatments. The first was a test predicting which men are likely to benefit from abiraterone and enzalutamide, by identifying cancers with multiple copies of the androgen receptor gene, which many prostate cancers rely on to grow. The other was a three-in-one test for advanced prostate cancer to identify which patients would benefit from treatment with PARP inhibitors, detect early signs of treatment failure and monitor drug resistance.
- In 2018, a major clinical trial led by the ICR and The Royal Marsden was the first to show that immunotherapy could benefit certain patients with advanced prostate cancer, including some men who had no other remaining treatment options.
- In 2018, a study involving more than 140,000 men identified 63 new genetic variants linked to prostate cancer. ICR researchers developed a new test able to detect these variants along with more than 100 that were already known. The test can predict which men are most at risk of developing the disease during their lifetime.
- In 2018, ICR researchers identified 80 molecular weaknesses in prostate cancer that could be targeted by drugs, opening up 60 new potential treatment strategies.

- In 2018, the ICR and The Royal Marsden delivered the first ever treatment in the UK using a Magnetic Resonance Linear Accelerator (MR Linac) machine. The MR Linac is the first technology in the world to simultaneously generate MRI images and deliver X-ray radiation beams, allowing radiotherapy to be adjusted in real time and delivered more accurately and effectively than ever before.
- In 2019, ICR researchers discovered that mutations in the retinoblastoma gene (already linked to cancer of the retina) are linked to poor survival and relapse in prostate cancer.
- In 2019, ICR researchers presented findings from the IMPACT study, which showed that annual PSA tests were more likely to pick out life-threatening forms of prostate cancer in men carrying a BRCA2 gene fault than in non-carriers.
- In 2019, a major study co-led by the ICR showed that a protein called androgen receptor splice variant 7 (AR-V7) – which is associated with advanced prostate cancer – begins to be expressed after hormone therapy as a mechanism of resistance. Preventing AR-V7 expression could lead to better patient outcomes.
- In 2019, results from the RADICALS-RT trial, led by Professor Parker, showed that men with prostate cancer could safely avoid routine radiotherapy after surgery, sparing them from adverse side effects.
2020s
- In 2020, the FDA approved the drug olaparib for some men with advanced prostate cancer as a result of the PROfound trial, co-led by the ICR’s Professor de Bono. This marked the first time that a drug was approved for cancers with faulty DNA repair genes beyond BRCA defects.
- In 2021, ICR scientists were part of a research team that revealed how gut bacteria contribute to the progression of advanced prostate cancers and their resistance to hormone therapy.
- In 2021, research as part of the IMPACT study confirmed that men who inherit an increased risk of cancer through ‘Lynch syndrome’ – a genetic condition that increases the risk of developing several cancers – could benefit from annual PSA testing from the age of 40.
- In 2022, new long-term findings from the radiotherapy arm of the STAMPEDE trial confirmed that delivering radiotherapy to the prostate, alongside the standard hormone therapy, could extend survival by an average of two years in some men with advanced prostate cancer.
- In 2022, the Medicines and Healthcare products Regulatory Agency (MHRA) approved 177Lu-PSMA-617, a highly targeted radioactive drug, for some patients with prostate cancer. Professor de Bono co-led the phase III trial, VISION, which led to this approval.

- In 2022, the ICR and The University of Cambridge developed a comprehensive tool, CanRisk-Prostate, which combines information on an individual’s genetic and family history to predict their risk of developing prostate cancer.
- In 2023, results from the UKGPCS study uncovered a link between a person’s family history of prostate cancer and their age at diagnosis.
- In 2023, the ICR, The Royal Marsden and RM Partners West London Cancer Alliance developed the ‘Man Van’, an innovative targeted outreach programme to improve healthcare access for men over the age of 45 from groups who are less likely to receive regular health checks. The research programme aimed to speed up the detection of prostate cancer.
- In 2023, ICR researchers showed that blocking signals used by prostate tumours to hijack white blood cells can reverse drug resistance. In a clinical trial led by Professor de Bono, combining AZD5069 (an experimental drug that prevents myeloid cell recruitment to tumours) and enzalutamide shrank tumours or halted growth in 24 per cent of patients with advanced prostate cancer.
- In 2023, olaparib was recommended by NICE as a treatment for NHS patients in England and Wales with early-stage prostate cancer, caused by faulty BRCA genes.
- In 2024, a later finding from the RADICALS-HD trial, led by Professor Chris Parker, found that radiotherapy alone is effective for low-risk prostate cancer post-surgery, while two years of hormone therapy benefits higher-risk patients.
- In 2024, the PACE-B trial, led by Professor Nicholas van As, showed that stereotactic body radiotherapy – which gives radiotherapy from many different angles around the body – is as effective when delivered in just five sessions, as standard radiotherapy for localised prostate cancer. The approach cuts treatment time by 75 per cent and minimises damage to healthy tissue.
- In 2024, ICR researchers worked out a way of predicting how long a prostate cancer patient will continue to respond to olaparib using a simple blood test to detect particular markers.
- In 2024, researchers discovered a genetic aberration found in some prostate cancers that makes them more vulnerable to PARP inhibitors which could enable more men to be treated with olaparib.
- In 2025, ICR researchers used an imaging technique to predict which patients are likely to respond to radium-223, a standard treatment for advanced prostate cancer that has spread to the bones.

- In 2025, researchers at the ICR showed that the drug NXP800, discovered at the ICR and currently in clinical trials for ovarian and bile duct cancer, slowed the growth of prostate cancer cells, including in cancer cells that are resistant to the hormone therapy enzalutamide.
- In 2025, the ICR’s BARCODE-1 study showed that a simple spit test using DNA from saliva is more accurate than PSA blood tests at identifying men at high risk of prostate cancer. The test has the potential to revolutionise screening by reducing unnecessary biopsies and treatments.
- In 2025, findings from a team of researchers at the ICR, led by Dr Adam Sharp, showed that a combination of two targeted drugs – fadraciclib and either ipasertib or capivasertib – not only slowed tumour growth but also triggered prostate cancer cell death, which may better prevent the development of resistance to treatment.
- In 2025, the latest results from the IMPACT study showed that men with BRCA1 mutations are more than three times as likely as non-carriers to have aggressive prostate cancers. On this basis, ICR scientists are calling for these individuals to be offered an annual PSA test.
- In 2025, an innovative study led by Dr Amanda Swain uncovered two genes that promote the formation of prostate cancer. These genes activate a signalling pathway that plays a vital part in the growth, division and death of cells, and is frequently mutated in prostate cancer.
Our pioneering research is transforming the outlook for men with prostate cancer. But some prostate cancers remain difficult to treat. That's why we urgently need better ways to detect prostate cancer earlier, predict drug resistance, and develop smarter, more personalised treatments. By supporting us today, you can help our scientists make more groundbreaking discoveries to help every man with prostate cancer live longer, healthier lives: