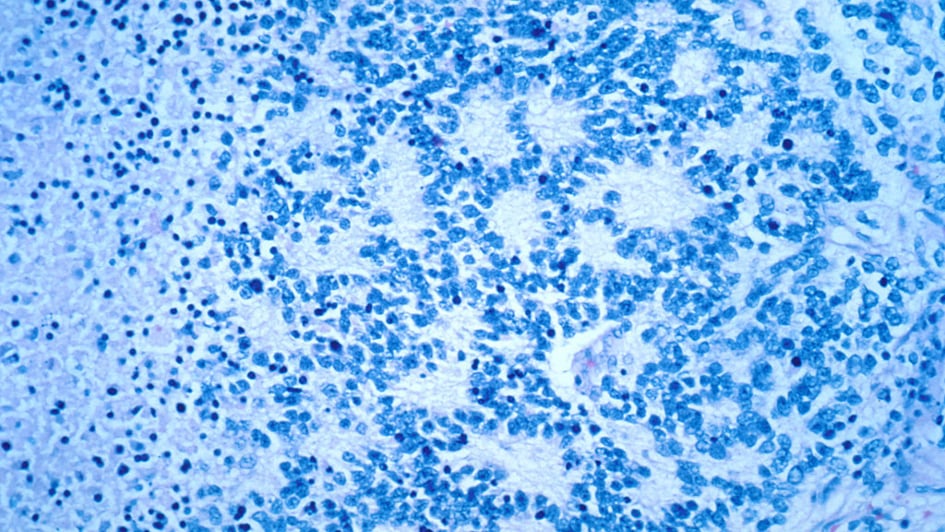
Image: Neuroblastoma rosettes. Credit: Dr. Maria Tsokos, National Cancer Institute [Public domain].
An aggressive form of the childhood cancer neuroblastoma could be treatable with two cancer drugs currently used in the treatment of colon and ovarian cancer, a study led by researchers at The Institute of Cancer Research, London, suggests.
A team led by researchers at the ICR modified neuroblastoma cells in the lab to silence a gene called ATRX, mutations to which are associated with a chemotherapy resistant form of the disease which is often fatal in children.
These ATRX-deficient cells were particularly sensitive to a combination of the drugs olaparib and irinotecan, which killed cancer cells by preventing DNA repair.
ATRX-deficient tumours in mice were also sensitive to the double treatment, including one derived from a child’s neuroblastoma tumour.
The research, published in the journal EBioMedicine, describes a new model for studying this aggressive form of neuroblastoma, and could lead to a new way of treating it.
The ICR is an internationally leading research centre in the study of childhood cancers and cancers in children, teenagers and young adults.
Find out more
Targeting DNA damage in aggressive childhood cancer
DNA damage is the underlying cause of cancer – but it is also a key weakness of cancer cells that can be exploited for treatment.
Knowing that the ATRX gene helps regulate DNA damage repair in healthy cells, the researchers reasoned that blocking other routes of DNA repair in neuroblastoma could leave cancers with ATRX mutations with a fatal level of DNA damage.
Using a gene editing technique called CRISPR, they first silenced ATRX in neuroblastoma cells, to generate a new model of the disease they could study in the lab.
They saw that ATRX-mutant neuroblastoma displayed key faults in a DNA damage repair mechanism called homologous recombination, which repairs double-strand breaks in DNA.
The researchers tested nearly 400 compounds that inhibit DNA repair in cancer cells, as well as DNA-damaging chemotherapy drugs.
They saw that ATRX mutant neuroblastoma cells were sensitive to a cancer drug called olaparib, which blocks an enzyme involved in DNA repair.
The drug is already used as a treatment for a range of adult cancers and is being studied in clinical trials for other forms of cancer in children.
Olaparib treatment was particularly effective when combined with the chemotherapy irinotecan, because it interfered with the cancer’s already weakened DNA damage repair mechanisms and pushed the cancer cells beyond repair.
Irinotecan and olaparib are already being used to treat cancer in adult patients, so the combination could be rapidly rolled out to treat children if clinical trials are successful.
This work was supported by a range of funders including the charities Christopher’s Smile, Neuroblastoma UK and Cancer Research UK.
The support and dedication of our family charity partners, who have been touched by cancer, is crucial in driving forward our work to better understand and treat childhood cancers.
Using readily available treatments for aggressive childhood cancer
Study leader Professor Louis Chesler, Professor of Paediatric Cancer Biology at the ICR and Consultant at the Royal Marsden hospital, said:
“ATRX-mutant neuroblastoma is a difficult to treat childhood cancer and there is a real need to identify new treatment strategies.
“Our research showed that combining two readily available cancer drugs, olaparib and irinotecan, could be an effective treatment for this form of the disease. Both drugs are already used as treatments for adult cancers, so if future trials of this combination are successful, they could be available as treatments relatively quickly.”
.tmb-propic-md.jpg?Culture=en&sfvrsn=c25d2b2f_9)
 .
.