
Image: Magi surrounded by her family. Credit: Magi Coad
Continued progress in cancer research means more and more people with advanced cancer are defying previous expectations and living for longer, with a better quality of life.
Even for those with cancers deemed incurable, new innovative and personalised treatments can help stop or slow the growth of the disease and give patients more time – sometimes with no evidence of disease.
But this is not yet the case for every patient – particularly those diagnosed with types of cancer that are rare or difficult to treat.
Here at The Institute of Cancer Research, we are working tirelessly to develop smarter, kinder treatments that can make even advanced cancer a manageable disease in the long term, and one that is more often curable.
We spoke to five people who received devastating cancer diagnoses, but after responding well to treatment are now looking to the future.
"I was told to get my affairs in order"
Magi Coad, 64, from Cornwall, was diagnosed with bowel cancer on New Year’s Eve 2019 and had surgery to remove it in February 2020. Within months she was told it had spread and that it was unlikely she’d make it to the end of the year. But then she started immunotherapy and saw amazing results:
“My first round of chemotherapy began just after lockdown started in March 2020, and I finished my treatment in late June. Everything was looking good, and I planned to go back to work as an office manager for a company that looks after people with learning disabilities and autism.
“But in July I was feeling really rubbish, so I went back to my oncologist and she scanned me. In early September she said, ‘Go home and get your affairs in order.’ The bowel cancer had spread to my peritoneum, my liver and my Iung. I was told I probably wouldn’t see Christmas, but that I could have immunotherapy as palliative care, to manage any pain and symptoms.
“In late September 2020 I was given my first dose of an immunotherapy drug called nivolumab.
“I had a few issues with side effects early on but here I am three years later, still on treatment - but with no liver or lung tumours, and no significant growth elsewhere. I’m now back to work full time and living a normal life – I get tired occasionally, but I can deal with that.

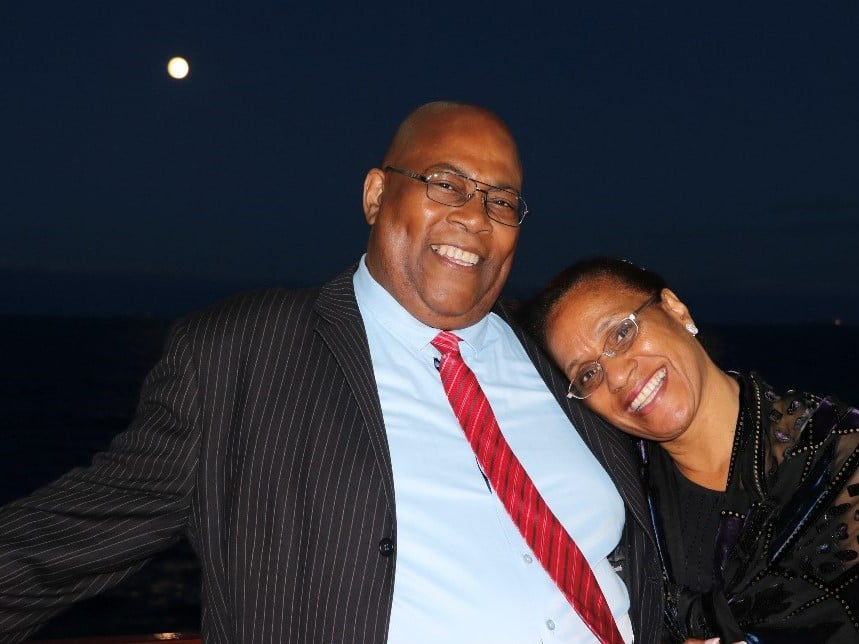
Magi with her husband Vern. Credit Magi Coad.
“I’m 64 and am a wife, mum and a grandmum. We’re a large family and enjoy each other’s company. I’m also quite a positive person, and dare I say it, quite stubborn sometimes. So when I was told I wouldn’t see Christmas I just held on to the fact that they were still offering me treatment, even if it was palliative.
“I have scans every three months now. There is anxiety before them, but they’re a part of my life now. I don’t expect anything to show up.
“I was told that immunotherapy would give me more time and I was willing to take the opportunity for any extra time at that point - anything would have been a bonus. But the outcome of my treatment has just been amazing.”
We are making exciting advances against cancer, which are helping people live longer and better. But to continue discovering smarter, kinder treatments, we need your ongoing support. A monthly gift from you will support our research over several years, so it has the maximum possible benefit for people with cancer.

Image: Alfred Samuels. Credit: Alfred Samuels
"It’s not just about surviving – it’s about so much more"
When Alfred Samuels, 66, from London was diagnosed with advanced prostate cancer in 2012, he felt as if his world had fallen apart overnight. Doctors said surgery wasn’t an option for him because the cancer had spread beyond his prostate, and he started to lose hope. But then he joined a clinical trial and began treatment with abiraterone, a drug discovered and developed by ICR scientists, which is now extending the lives of thousands of men worldwide.
Twelve years later, Alfred says: “Abiraterone has saved my life and I am grateful for that. But not everyone is as fortunate as I was to get on that trial and respond to the drug as well as I did. We need more treatments like abiraterone. Drugs that enable people to live their lives with cancer, and live them well. It’s not just about surviving - it’s about so much more.
“I’m still being treated with abiraterone and Zoladex, a hormone therapy, and I live differently now. My work is focused on being a patient advocate. I try to help men come to terms with their diagnoses and the effects of long-term treatment on their bodies.
Alfred with his wife Grace. Credit: Alfred Samuels
“Over several years now I have given advice, support, awareness and education to men who have unfortunately followed a similar path. I want to be a voice of hope, inspiration and motivation for men with this disease that disproportionately affects black men, so I use my experience to engage with different cultures and ethnic groups.”

Image: Karen with her swimming friends. Credit: John Angerson
"Living well with cancer is my reality"

Image: Karen with her grandsons. Credit: John Angerson
“Living well with cancer is my reality. I spend most of my time with my family – I’m very involved and do pick-ups from school and nursery. Five years ago I got my little dog Poppy, and I love going on walks with her. I also started wild swimming - it makes me feel so well and alive.
The chemotherapy drugs and targeted drug work together and keep the cancer at bay. Every four months I go for a routine CT scan and currently there is no sign of cancer.”
In our Centre for Cancer Drug Discovery our scientists are tackling cancer’s lethal ability to evolve resistance to treatment. Here, we aim to develop a new generation of drugs that will make the difference to the lives of millions of people with cancer. Learn more about this vital work and how you can support us:
Image: Steve Clark. Credit: Steve Clark
"I want to give people hope"
Steve Clark, 59, from Berkshire, was diagnosed with advanced bowel cancer in 2013. Four years later, he set up the non-profit organisation Strive for Five to give hope to people with stage 4 cancer.
In 2023 he updated the name to Strive for Five and Beyond to recognise that more and more people are living fulfilling lives beyond what he calls the ‘magic five-year mark’.
It’s now been more than ten years since his diagnosis and he’s living an active and full life:
“In May 2013, when I was 49, I was diagnosed with stage 4 bowel cancer and fast-growing secondary tumours in my liver and both lungs. I had an operation to remove the large primary tumour in my bowel and then intense chemotherapy called FOLFIRI, plus a targeted drug called bevacizumab for six months.
“The treatment was very successful – afterwards my liver and one lung were clear, the other lung had just three small spots, so the surgery scheduled to remove the lung tumours was cancelled. I felt very lucky.
“I started on long-term maintenance chemotherapy in January 2014 to keep the cancer at bay, which consists of an infusion of bevacizumab, followed by capecitabine tablets. I’ve been told I’ll be on this for life and that’s fine with me as it’s doing such a great job controlling the cancer.
“In October 2016, the cancer returned in my lymph nodes which was treated with chemo. In May 2017, another recurrence in my lung was successfully treated with radiofrequency ablation (RFA) which burns out the tumour without the need for major surgery.
“Initially, whenever I asked my oncologist about my prognosis he always said it was hard to see beyond the next 12-18 months, I viewed this as a target to beat and I’ve kept beating it.
“I’ve just passed the 10-year mark, proving that the stats aren’t predictors of individual survival. My oncologist is much more optimistic about things now and thinks I can look forward to a long future!
“I’m in my late 50s now and looking forward to a long and fun-filled life. I’m an active person, run a small business, and I’ve drawn up a bucket list to make the most of my time with friends and family. I focus a lot of my time trying to help others with this disease through Strive for Five.

Image: Steve on holiday. Credit: Steve Clark
“Since my diagnosis I’ve travelled throughout Europe and been to the US several times since. I’ve even been into the Arctic Circle, to Bali on a yoga holiday and travelled into the Borneo rainforest to see the orangutans and sun bears! This isn’t the sort of activity people usually associate with stage 4 cancer, and I hope by sharing my story I can help change those perceptions and give people hope.”
Image: Karen Dowds with her grandchildren. Credit Karen Dowds
"I never thought I’d see my daughter reach eighteen"
Karen Dowds, 52, who lives in Fife, Scotland, first went to the GP in August 2018 with excruciating pain in her right shoulder blade. She was eventually diagnosed with stage 4 lung cancer and told it had spread to various places, including her brain.
“My eldest sister was with me at my pre-treatment consultation, and asked about my prognosis, but I didn’t want to know.
“When I first got my cancer diagnosis I’d never even heard of immunotherapy, but it was the only treatment that was offered to me – no chemo and surgery wasn’t an option as there were too many areas the cancer had spread to.
“I started on pembrolizumab, a type of immunotherapy, in June 2019.
“By November that year the main tumour in the lung had shrunk. Only one lesion in the brain was seen in the scan and it had also shrunk! The other areas the cancer had spread to, including the groin, lymph gland and my abdomen had all returned to normal.
“My treatment ended in June 2021. My last scan in November 2022 showed only residual scarring in the lung and calcified lesions in the brain. No tumours.
“I’m still processing it all – that all it took was one treatment and now there’s only scarring where the cancer was. I know I’ve been incredibly lucky – my oncologist warned me about survivor’s guilt, but it was such a strange experience.
“Just before I was diagnosed I had a conversation with a surgeon who was going to do a biopsy, and I was in bits. He gently asked me what I was so upset about and I replied: ‘You’re about to determine the future of my 13-year-old daughter.’
“Well now my daughter has just turned 18. I never thought for one minute I would see that – or see my son reach 30.
“In the past five years I’ve also seen my two grandchildren being born – they are such a blessing. I just wish everyone could respond to cancer treatment the way I have.”
Bringing more hope to people with cancer
We have made huge strides in research and treatment for people with cancer, extending their lives and improving their quality of life. But we want to make stories like this a reality for more people with advanced cancer. Our work is ambitious – and we need your ongoing support to help continue making more discoveries and saving more lives.
A regular monthly donation will help us to take on new challenges, safe in the knowledge of sustained funding into the future. It gives us the regular, predictable support we need to make real progress.
Please support us today.


