CLOSED: The Role of Early Plasma Cell Infiltration in Breast Cancer Immune Responses
Application closing date: 16/11/25
Project background
Current understanding of immune tolerance in cancer focuses on established tumours, but the critical early events that allow developing cancers to evade immune surveillance remain poorly understood. By the time breast cancers are clinically detectable, tolerance mechanisms are already established, making it difficult to study their origins.
The BRCA1/p53-deficient (BP) in vivo cancer model closely recapitulates human hereditary breast cancer development, progressing from normal mammary tissue through ductal atypia to invasive cancer (Molyneux et al. 2010)). Importantly, preliminary analysis of early lesions in this model reveals activation of the type I interferon pathway, likely driven by genomic instability in atypical cells (Bach et al. 2021). This early interferon signalling creates a pro-inflammatory environment that coincides with immune cell recruitment.
A striking observation from the BP model is that plasma cells infiltrate mammary tissue at the very first signs of atypia—well before invasive cancer appears. This early timing suggests plasma cells are among the first immune responders to genomic instability, positioning them to actively shape initial immune-cancer interactions during malignant transformation.
Previous work demonstrated that cancer-associated fibroblasts (CAFs) activate STING signalling in response to genomic stress from neighbouring cells, producing sustained type I interferon (Arwert et al., 2020). The early activation of type I IFN pathways observed in developing BP lesions provides a mechanistic link to plasma cell recruitment, as type I interferons create tissue environments that support plasma cell survival whilst potentially establishing immunosuppressive cascades.
The central question is whether early plasma cell infiltration represents effective immune surveillance that subsequently fails, or whether these cells actively promote tolerance from the outset. Understanding this distinction could reveal whether plasma cells are part of the problem or part of a solution, with significant implications for early intervention strategies in breast cancer development.
Project aims
- Characterise the temporal dynamics and functional impact of early plasma cell infiltration during breast cancer development, testing whether plasma cell presence correlates with reduced T cell infiltration and enhanced tumour progression in the BP model.
- Investigate the role of CAF-derived STING/type I IFN signalling in establishing plasma cell niches by testing whether STING activation is necessary for plasma cell recruitment and whether blocking this pathway prevents tolerance establishment.
- Determine the functional consequences of early plasma cell presence and test whether modulating plasma cell recruitment or function affects immune surveillance of pre-malignant breast tissue.
Further details & requirements
This project aims to understand the role of early plasma cell infiltration in breast cancer immune responses, investigating whether these cells promote immune tolerance or represent failed immune surveillance during the earliest stages of malignant transformation.
Aim 1: Map temporal relationships between genomic instability, type I IFN activation, and plasma cell recruitment
The BP model will be aged to capture the full spectrum from normal mammary tissue through early atypia to established lesions. Animals will be sacrificed at defined timepoints to collect tissue representing different developmental stages.
Developmental stage analysis using multiplex immunohistochemistry to simultaneously detect plasma cells (CD138, BLIMP1), type I IFN pathway activation (ISG15, IRF7), genomic instability markers (γH2AX, 53BP1), and immune cell populations (eg F4/80, CD4, CD8 T cells, B cells). This will establish the precise temporal sequence of events during early development.
Quantitative analysis using automated image analysis to correlate plasma cell density with markers of genomic damage and immune activation across multiple BP animals and developmental stages.
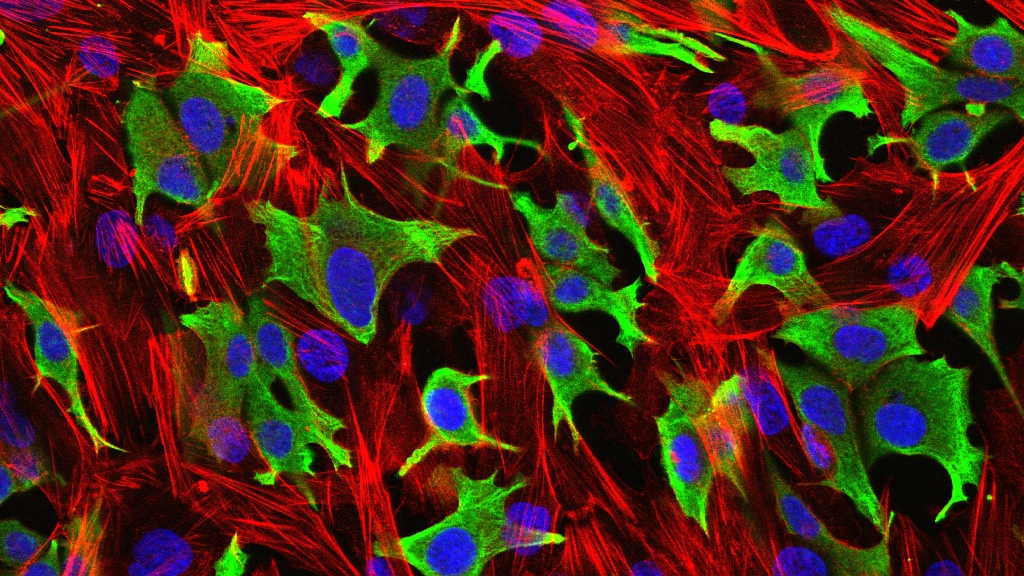
Spatial relationship analysis using established 7-colour immunofluorescence panels to determine whether plasma cell density correlates with T cell exclusion patterns or altered T cell activation states. Neighbourhood analysis will identify which cell types preferentially associate with plasma cells.
Flow cytometry validation of tissue dissociation protocols to quantify plasma cell numbers and phenotypes across developmental stages, providing complementary data to spatial analysis.
Spatial transcriptomics using 10x Visium HD to map gene expression patterns across developing lesions, identifying signatures associated with plasma cell recruitment and type I IFN activation. Integration with our existing spatial datasets will provide comprehensive molecular maps of early immune dynamics.
Aim 2: Investigate the role of CAF-derived STING/type I IFN signalling in establishing plasma cell niches
Genetic approaches will test STING pathway requirements for plasma cell recruitment:
Long-term strategy: BP x STING knockout crosses initiated in Year 1 for analysis in Years 3-4, providing definitive genetic evidence
Pharmacological validation using STING inhibitors (H-151, C-176) administered during early lesion development to test whether acute STING blockade prevents plasma cell establishment.
Type I IFN receptor blocking using αIFNAR antibodies during early development to test whether type I IFN signalling is required for plasma cell establishment, distinguishing STING-dependent versus independent pathways.
In vitro mechanistic studies using mammary CAFs stimulated with cocultured with BP model organoids which drives STING activation, to test direct effects of STING activation on factors that support plasma cell recruitment and survival.
Aim 3: Determine functional consequences of early plasma cell presence
B cell and plasma cell depletion studies using αCD20/ αCD138 antibodies during early BP development to prevent plasma cell formation entirely, monitoring effects on immune cell infiltration patterns and lesion progression.
Functional immune analysis using flow cytometry to assess T cell activation states, proliferation, and cytotoxic potential in plasma cell-depleted versus control environments. Focus on activation markers (CD69, IFNγ, granzyme B) and exhaustion markers (PD-1, TIM-3).
Mechanistic investigation using single-cell RNA sequencing of immune populations from plasma cell-depleted versus control lesions to identify transcriptional changes in T cell populations and other immune cells.
Disease progression analysis monitoring whether plasma cell modulation affects the rate of transition from pre-malignant lesions to invasive cancer, providing functional evidence for their role in immune escape mechanisms.
Clinical validation in collaboration with Dr Elly Sawyer, mining DCIS datasets to identify plasma cell signatures that predict progression to invasive cancer. These human-derived signatures will be validated in the BP model and used to prioritise therapeutic targets, testing whether interventions targeting patient-relevant pathways prevent lesion progression in the mouse model
Computational Analysis
Working in collaboration with Dr Syed Haider's team, the student will analyse spatial transcriptomics data to identify neighbourhood relationships between plasma cells, CAFs, and T cells. Machine learning approaches will identify gene expression signatures predictive of immune tolerance establishment.
Expected Outcomes
- Temporal framework establishing when and how plasma cells are recruited during early breast cancer development in relation to genomic instability and type I IFN activation
- Mechanistic understanding of STING pathway requirements for plasma cell recruitment, distinguishing stromal versus immune cell contributions
- Functional characterisation determining whether plasma cells promote immune tolerance or represent failed surveillance attempts
- Therapeutic targets for preventing tolerance establishment through modulation of plasma cell recruitment pathways
- Translational insights with potential relevance to human breast cancer prevention and early intervention strategies
This project addresses fundamental questions about early immune-cancer interactions using a clinically relevant model system with established technical capabilities. The work could establish plasma cells as previously unrecognised players in early tolerance establishment whilst identifying new prevention strategies.
Candidates must have, or be on track to receive, a First- or Upper Second- class Honours degree (or a Masters) in Biological Science and have experience in Cancer Biology, and must have a basic knowledge of Tumour Immunology.
ARWERT, E. N., MILFORD, E. L., RULLAN, A., DERZSI, S., HOOPER, S., KATO, T., MANSFIELD, D., MELCHER, A., HARRINGTON, K. J. & SAHAI, E. 2020. STING and IRF3 in stromal fibroblasts enable sensing of genomic stress in cancer cells to undermine oncolytic viral therapy. Nat Cell Biol, 22, 758-766.
BACH, K., PENSA, S., ZAROCSINCEVA, M., KANIA, K., STOCKIS, J., PINAUD, S., LAZARUS, K. A., SHEHATA, M., SIMÕES, B. M., GREENHALGH, A. R., HOWELL, S. J., CLARKE, R. B., CALDAS, C., HALIM, T. Y. F., MARIONI, J. C. & KHALED, W. T. 2021. Time-resolved single-cell analysis of Brca1 associated mammary tumourigenesis reveals aberrant differentiation of luminal progenitors. Nat Commun, 12, 1502.
MOLYNEUX, G., GEYER, F. C., MAGNAY, F. A., MCCARTHY, A., KENDRICK, H., NATRAJAN, R., MACKAY, A., GRIGORIADIS, A., TUTT, A., ASHWORTH, A., REIS-FILHO, J. S. & SMALLEY, M. J. 2010. BRCA1 basal-like breast cancers originate from luminal epithelial progenitors and not from basal stem cells. Cell Stem Cell, 7, 403-417