CLOSED: Comprehensive multi-omics profiling of “islands of resistance” tumour cells to uncover aromatase inhibitor resistant subclones in oestrogen receptor positive breast cancer
Application closing date: 16/11/25
Project background
Over 80% of breast cancer (BC) patients in the developed western world have oestrogen receptor (ER)–positive disease; their treatment normally includes surgery and adjuvant endocrine therapy, and sometimes chemotherapy which greatly improves survival outcome (1). In postmenopausal women, the most effective endocrine therapy agents are aromatase inhibitors (AIs). Many patients recur because of de novo or acquired resistance to AI.
Currently, abemaciclib is approved for high-risk, node positive hormone receptor (HR)+/HER2- early BC in US and UK, supported based on the results from the phase 3 MonarchE randomised controlled trial (2). HR+/HER2+ BCs are molecularly heterogeneous with 30% of them are HER2-Enriched (HER2-E). We showed that HR+HER2-E is characterised by an immune-activated stroma with elevated tumour infiltrating lymphocytes, lower expression of luminal-related genes than the HR+/Luminal subtypes and benefit greatly from anti-HER2 therapies but poorly from endocrine therapy (ET) (3).
Resistance to endocrine therapies has been mainly studied in HR+/HER2- BC, but those mechanisms might differ between HER2+ and HER2- tumours, in part due to the differential distribution of intrinsic subtypes within each BC subgroup. Cells within a single tumour can be genetically diverse and respond differently to treatment. Even in tumours with good response to treatment, there may be a few resistant cells that remain growing and might be responsible for recurrences if not removed or killed by other methods.
The PeriOperative Endocrine-Therapy for Individualised Care (POETIC) trial (4) provides a framework to study endocrine resistance mechanisms in a large set of ER+ HER2+ and HER2- BC patients. The objective of this PhD project is work on method(s) to isolate these resistant tumour cells and discover genomic changes that are specific to these resistant cells. This will allow us to understand why these cells do not respond to treatment and may allow additional personalised treatment targeting these resistant cells.
Project aims
- To determine whether the ER+ Ki67 (proliferating) persistent cells are different at a genomic (either genetic or epigenetic) from the non-proliferating cells isolated after peri-operative AI
- To determine whether those genomic markers in the Ki67 persistent cells after peri-operative AI at 2 weeks are found in local and distant recurrent disease?
- To identify new drug candidates by comparative analyses with the genomic profiles from target ER+ cell lines treated with investigational drugs in AstraZeneca
Further details & requirements
Mechanisms of resistance to aromatase inhibitors (AIs) vary between patients; a rational application of the emerging large number of targeted agents against resistance mechanisms that are present in individual tumours requires novel clinical approaches. We propose to analyse data from the POETIC (Peri-Operative Endocrine Therapy – Individualising Care) study (4). POETIC was an open-label, multicentre, parallel-group, randomised, phase 3 trial (done in 130 UK hospitals) in which 4480 postmenopausal women aged at least 50 years with WHO performance status 0–1 and hormone receptor-positive, operable breast cancer were randomly assigned (2:1) to POAI (letrozole 2·5 mg per day orally or anastrozole 1 mg per day orally) for 14 days before and following surgery or no POAI (control). Adjuvant treatment was given as per UK standard local practice. In this cohort, we found that KI67 levels and changes in the levels after perioperative AI treatment was associated with time to recurrence (TTR) and overall survival (OS) (4). The Ki67 value was measured using the standardised visual score method and they were as follows: all stained and unstained invasive tumour nuclei were counted in at least 5 high-power fields (i.e., the most representing field); the Ki67 staining index was calculated as the total number of stained nuclei counted/total number of all invasive nuclei counted.
Intratumor heterogeneity of Ki67 expression after neoadjuvant endocrine therapy is suggested to be associated with poor outcomes and resistance to treatment but datasets and techniques to identify genomic differences between the resistant and sensitive subclones has been limited. The key overall question is whether those persistent Ki67 cell populations identify clonal populations that will grow out under continued treatment pressure and drive the growth of micro-metastases to reveal themselves as recurrent disease. This question will be broken down into three sub questions.
Are the ER+ persistent proliferating cells different at a genomic (either genetic or epigenetic) from the non-proliferating cells at 2 weeks?
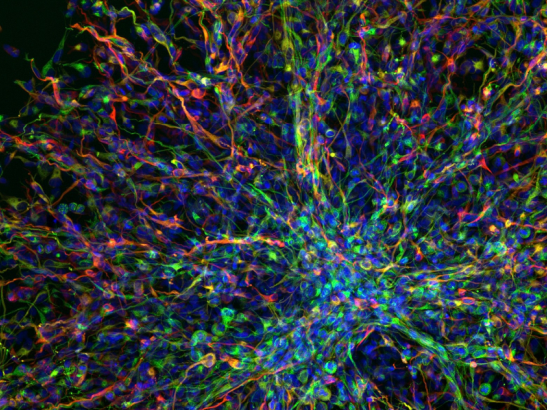
Based on our pilot project, using multi-parameter fluorescence-activated cell (FACS) sorting of 26 AI treated FFPE POETIC samples (at 2weeks) enabled the separation of de novo AI-resistant from sensitive cell populations and whole genome sequencing revealed a higher mutational burden in the AI-resistant populations at the time of disease presentation (5). This suggests that interrogation of the mutational differences between the proliferative and non-proliferative cells may allow identification of putative drivers of resistance in individual tumours. This FACS method provides an important bridge between approaches that are low cost , labour intentive but give a limited view of tumour heterogeneity (needle microdissection) and those that are high-cost but provide full view of heterogeneity (spatially resolved single cell sequencing).
As single-cell omics techniques on FFPE tissues are rapidly evolving, we will explore emerging approaches such as Cyclic Immunofluorescence, 10x Visium, Nanostring Digital Spatial Profiling, and/or CosMx SMI. If this proof-of-concept study is successful, we will extend the workflow to additional patient samples. To provide a complementary layer of spatial context, we will apply digital pathology approaches, including high-throughput image analysis and machine learning, to quantify morphological and biomarker-defined tumour subpopulations. Integration of digital pathology with spatial and bulk multi-omics will allow us to interrogate resistant clones within their native microenvironment, linking histological features with molecular profiles at scale.
We will assess whether resistant clones stratify by HER2 status or intrinsic subtype (PAM50 assay). A central question is whether genomic markers identified in Ki67-persistent cells at 2 weeks are also present in distant recurrent disease, and whether these differ from markers in locoregional recurrence.
POETIC provides a unique opportunity to address this. The protocol includes optional recurrence sample collection at the time of relapse. o date, 15 distant recurrence samples have been identified based on 5-year follow-up and are available for analysis. Additional locoregional recurrence and positive lymph node samples (supported by another project) will also be retrieved, enabling systematic comparison of genomic markers across primary, locoregional, and distant recurrences.
We will also investigate whether better treatment approaches can be identified for aromatase inhibitor–resistant clones. In collaboration with Translational Medicine and Bioscience colleagues at AstraZeneca, we will compare the genomic and phenotypic features of resistant clones with data from cell lines and patient-derived cancer models. This will allow us to test the activity of current AIs against next-generation endocrine therapies or novel therapeutic combinations. The findings aim to identify alternative therapeutic strategies, refine biomarkers for patient stratification, and define biological endpoints for adaptive (e.g., Bayesian) clinical trial designs.
By incorporating digital pathology, spatial omics, and bulk multi-omics, this PhD project will provide a multi-layered understanding of endocrine therapy resistance biology. Partnering with AstraZeneca will further enhance its clinical relevance by linking molecular resistance signatures to candidate therapies. The student will gain skills across computational and experimental domains, with a unique opportunity to learn how forward and reverse translation can inform the design of next-generation cancer trials.
- Funding is available for home students only
- Candidates must have a First or 2:1 Honours degree or a master’s in computer science, mathematics, engineering, statistics, or a related discipline.
- Academic knowledge of cancer biology, cell biology, digital pathology or analytical chemistry
- Strong presentation and communication skills
| [1] Sirvén MB, López-Knowles E, Zhu X, et al. Short-duration preoperative endocrine therapy alters molecular profiles to predict favourable outcome in ER+/HER2+ early breast cancer: a POETIC translational study. EBioMedicine. 2025 Aug;118:105823. doi: 10.1016/j.ebiom.2025.105823. Epub 2025 Jul 18. [2] Schuster EF, Lopez-Knowles E, Alataki A et al. Molecular profiling of aromatase inhibitor sensitive and resistant ER+HER2- postmenopausal breast cancers. Nat Commun. 2023 Jul 7;14(1):4017. doi: 10.1038/s41467-023-39613-z. [3] Early Breast Cancer Trialists' Collaborative G.: Aromatase inhibitors versus tamoxifen in premenopausal women with oestrogen receptor-positive early-stage breast cancer treated with ovarian suppression: a patient-level meta-analysis of 7030 women from four randomised trials. Lancet Oncol. 2022;23(3):382-92 [4] Martin M, Hegg R, Kim SB, et al.: Treatment with adjuvant abemaciclib plus endocrine therapy in patients with high-risk early breast cancer who received neoadjuvant chemotherapy: a prespecified analysis of the monarchE randomized clinical trial. JAMA Oncol. 2022 Aug 1;8(8):1190-1194. [5] Bergamino MA, López-Knowles E, Morani G, et al.: HER2-enriched subtype and novel molecular subgroups drive aromatase inhibitor resistance and an increased risk of relapse in early ER+/HER2+ breast cancer. eBioMedicine,2022. [6] I Smith, J Robertson, L Kilburn, et al.: Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial Lancet Oncol, 21 (2020), pp. 1443-1454 [7] Schuster ER, Zabalgo L, Perou CP, et al.: Multi-parameter FACS sorting identifies higher mutational burden in aromatase inhibitor resistant subclones in estrogen positive breast cancer at diagnosis San Antonio Breast Cancer Symposium; 2019 Dec 10-14; San Antonio, TX. Philadelphia (PA)2019. |