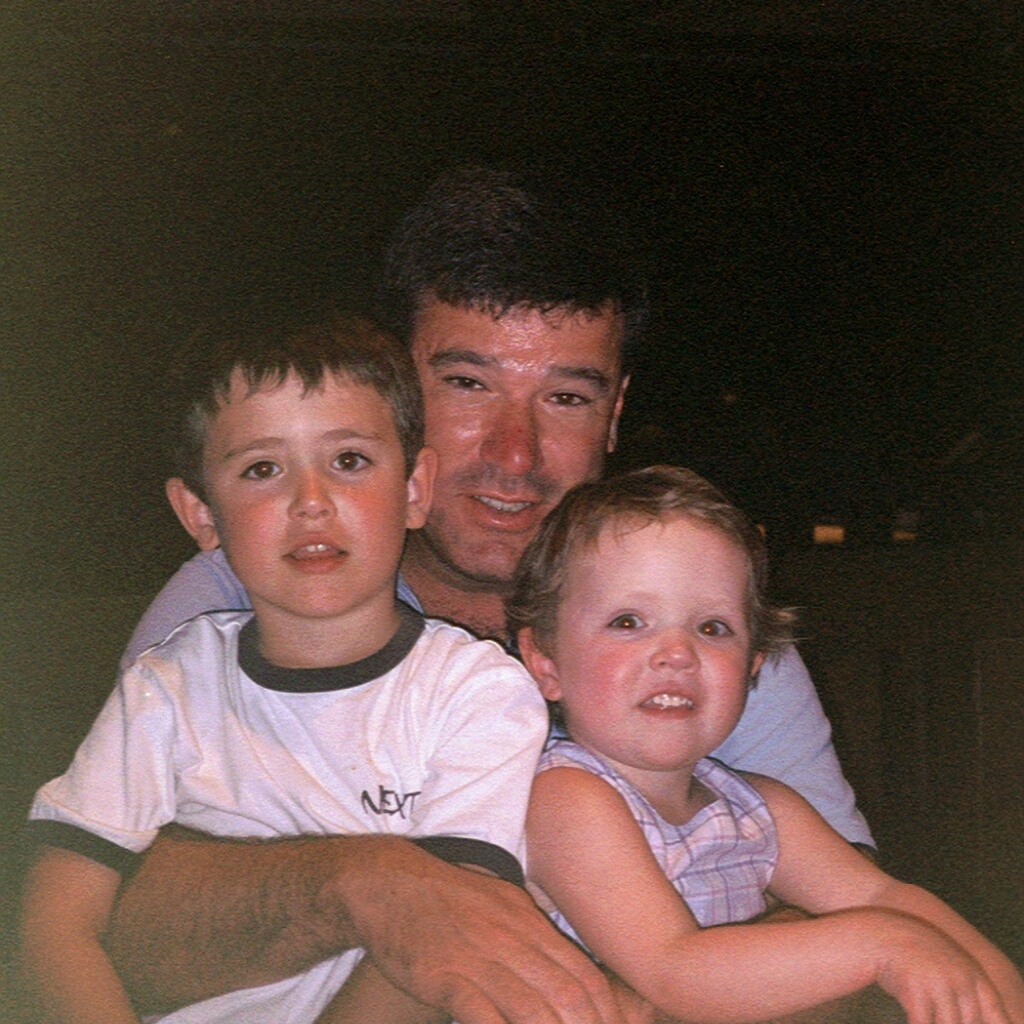
Diffuse midline gliomas (DMGs) are one of the most aggressive and hard-to-treat childhood cancers. These primary brain tumours, which are also sometimes called diffuse intrinsic pontine gliomas (DIPG), develop in the midline regions, including the thalamus, brainstem and spine, and most often affect children and young adolescents.
With a median survival of just 8–11 months, and only around 10 per cent of patients surviving beyond two years, DMGs present a devastating prognosis. Despite an ever-increasing understanding of the biology of these tumours, treatment options remain limited. Radiotherapy is currently the only standard of care – it may help temporarily slow tumour growth and improve symptoms, but it cannot offer a long-term cure.
A collaborative plan to accelerate drug development
In response to the urgent need, the 13th Paediatric Strategy Forum was convened by ACCELERATE – an international platform bringing together multiple stakeholders with a mission to accelerate therapeutic innovations for children and adolescents with cancer.
Held in Toronto last year, the forum brought together a collection of global stakeholders – including scientists, clinicians, patient advocates, pharmaceutical representatives and regulatory bodies – to establish a strategic framework for advancing DMG drug development for children and adolescents.
The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust played a significant role in the effort, with researchers Professor Chris Jones, Dr Julia Cockle, Dr Lynley Marshall and Dr Fernando Carceller, attending and presenting at the forum, contributing to discussions and workshops that are shaping the approach to childhood brain tumour therapy.
With biological discoveries opening new therapeutic avenues, stakeholders are pushing for a united response to progress treatments from the laboratory bench to the hospital bedside. The outcomes of the forum – including a prioritised list of therapeutic targets, recommendations for innovative clinical trial design and calls for greater collaboration between academia, regulators and industry – were summarised in a position paper published in the European Journal of Cancer earlier this year.
The role of the ICR and The Royal Marsden
The Institute of Cancer Research (ICR) and The Royal Marsden continue to be at the forefront of research efforts to take biological discoveries through to benefit children with aggressive cancers, such as DMG. For example, Professor Chris Jones’ laboratory will serve as the translational biology lead for BIOMEDE2.0 and TarGeT – the two major clinical trials for DMG – helping to guide how scientific findings are applied to the clinic.
As part of these efforts, there is increasing acknowledgment of the need to design more efficient clinical trials that produce sufficient evidence, more rapidly, for regulators to approve new treatments. This approach will help to ensure that promising therapies can reach children and young people as quickly and safely as possible.
Dr Marshall, who is also a consultant oncologist treating children and young people at The Royal Marsden, said: "We’re proud to be playing a leading role in international efforts to tackle a devastating childhood cancer. By turning cutting-edge science into targeted therapies and through collaboration with global partners and industry, we’re determined to bring better outcomes to children with DMG.”
New targets and new outcomes
One of the key outcomes from the forum was a call to identify and prioritise promising molecular targets for DMG treatment. Researchers at the ICR are already advancing this area, playing a central role in uncovering some of the genetic drivers of DMG – including mutations in a gene called ACVR1.
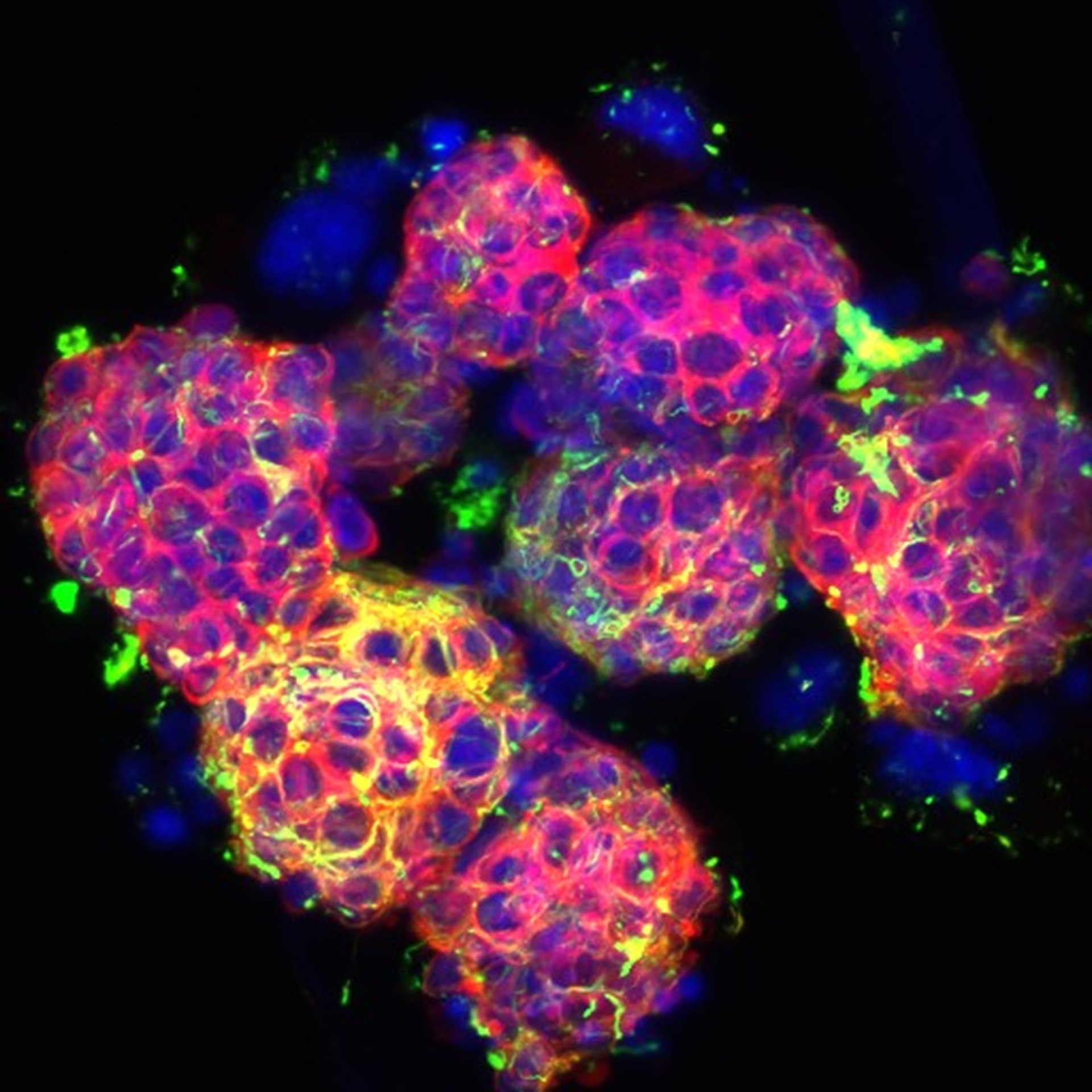
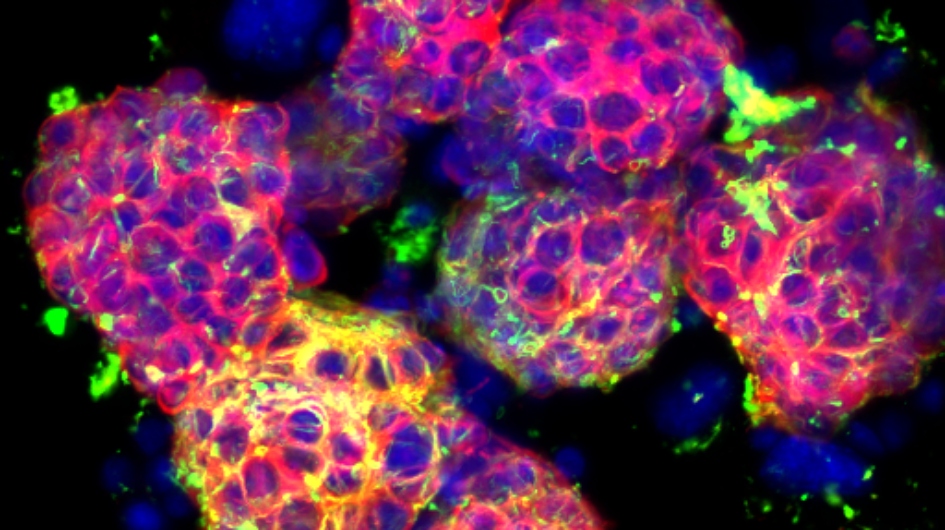
Found in about a quarter of DMG patients, mostly in younger children, the mutations cause the gene to become overactive, driving tumour growth and supporting its survival. Professor Jones and his team discovered the mutation in DMG in 2014 and have been working on the biological and preclinical assessments of the potential therapeutic target ever since.
While such findings offer promising new targets, translating them into effective therapies remains a challenge, requiring innovative approaches to drug delivery and close collaboration between stakeholders. At the ICR, this translational work is supported by the Brain Tumour Research-funded Centre of Excellence, which was established specifically to generate preclinical data for prioritising agents for clinical trials.
One potential small molecule drug, ONC201, has shown signs of effectiveness in some patients. It targets a dopamine receptor and the integrated stress response – pathways thought to be relevant in DMG. So far, the evidence for the drug’s effectiveness has mainly come from anecdotal reports and early-phase studies – randomised clinical trial data is still lacking.
A phase II study, BIOMEDE2.0, which will compare ONC201 with everolimus to gain a clearer insights into the drug’s effectiveness, is due to open in the UK for DMG patients. This research directly supports the forum’s call for more adaptive, internationally informed trials that can help accelerate access to new treatments.
Overcoming drug delivery challenges
While identifying and testing new therapies is critical, one of the most significant barriers to treating DMG is ensuring that drugs can actually reach the tumour. The blood-brain barrier – a naturally protective membrane preventing toxins and pathogens in the blood from entering the central nervous system – limits the ability of chemicals, drugs and biopharmaceuticals to reach brain tissue, including any tumours.
At the ICR, advances in new delivery techniques, such as a joint PhD project under Professor Jones and Professor Gail ter Haar, Professor of Therapeutic Ultrasound, exploring how focused ultrasound can temporarily open the blood-brain barrier, or packaging drugs in nanoparticles, are promising approaches that could revolutionise treatment.
Collaborative efforts to innovate in this space are essential to improving patient outcomes. Researchers at the ICR, including joint PhD projects under Professor Jones with Dr Gary Newton, Group Leader in Medicinal Chemistry, at the Cancer Research UK Children’s Brain Tumour Centre of Excellence and with Dr Gabriela Kramer-Marek, Group Leader in Preclinical Molecular Imaging, on photoimmunotherapy, are exploring how these delivery techniques could be integrated into future treatment strategies.
International, collaborative trials: a vision for the future
The forum emphasised the need for international trials to harmonise efforts across countries. Existing platform trials established by paediatric neuro-oncology associations, such as the Paediatric Neuro-Oncology Consortium (PNOC) in the US, the US-led but internationally collaborative Network for Neuro-oncology Clinical Trials (CONNECT) and Europe’s Innovative Therapies for Children with Cancer (ITCC) are leading the way. These innovative trial designs – which allow multiple treatments to be tested simultaneously within the same trial structure – allow new therapies to be tested quickly and efficiently.
However, these trials can be complex to run. Aligning the requirements of different regulatory authorities, ensuring standardisation of care across different health systems, providing consistent trial inclusion assessment and securing funding present major challenges.
Professor Jones, Professor of Childhood Brain Tumour Biology at the ICR, said: “We hope PNOC, CONNECT and ITCC, or other subsequent collaborations, will be a major advance in bringing novel agents and approaches to patients with DMG.”
Professor Jones is the Biology Lead for one of the CONNECT trials, called TarGeT, which will open soon in the UK. Like BIOMEDE2.0, TarGeT is designed to evaluate multiple emerging therapies for DMG using an adaptive platform trial structure. The aim is for these trials to be not only scientifically robust, but also aligned with regulatory requirements to ensure any promising treatments can move swiftly towards approval.
A call for continued collaboration
The success of these clinical trials and global platforms will continue to rely on international collaboration. By uniting the expertise of stakeholders across the globe, the shared goal of transforming outcomes for children with aggressive cancers, such as DMG, is possible. The outcome of the forum reflects the strength of collective action in tackling childhood cancer.
Professor Jones said: "The biological understanding of DMG has grown tremendously over the past decade. The 13th Paediatric Strategy Forum was crucial in reviewing emerging therapeutic targets and setting priorities for future research. While we’ve seen encouraging signs from drugs such as ONC201, robust clinical data are essential. Fortunately, the upcoming BIOMEDE2.0 and TarGeT trials in the UK, which the ICR and The Royal Marsden will play a vital part in, will provide critical insights."
With ongoing studies and evolving scientific insights, the future holds promise. The outcomes of the forum serve as both a call to action and a hopeful step towards reliable treatments and positive outcomes for children and families affected by DMG.