New research has provided insight into the biological mechanisms that may contribute to poor outcomes in certain cases of neuroblastoma – a cancer that develops in nerve tissue and primarily affects children.
A high-risk form of the disease that is progressive and difficult to treat is often associated with mutations in the ATRX gene, which controls the expression of multiple sections of the genome and plays a part in children’s development.
Using a range of techniques, the team, led by scientists at The Institute of Cancer Research, London, uncovered how common ATRX alterations affect the local interactions between cancer cells and the body’s immune cells, known as the tumour immune microenvironment (TIME).
By building on this information, researchers should be able to strengthen the understanding of why children with these mutations typically have less positive outcomes. The findings should also drive international efforts to correlate ATRX status more closely with response to the treatments currently given in clinical trials, with the long-term aim of developing more effective treatment regimens for this patient subgroup.
The study was primarily funded by Neuroblastoma UK and Cancer Research UK, and the findings were published in the journal Cancer Letters.
Treatment needs to be more tailored
Currently, all children with high-risk neuroblastoma – with risk being determined by the child’s age and the stage and genetics of the cancer – are treated in the same way. They all receive chemotherapy and a type of immunotherapy called anti GD-2 antibody.
However, the chance of survival for these patients is only about 50 per cent, showing that this treatment approach is often not effective. Among the children who tend to have worse outcomes are those with ATRX alterations, which affect about 10 per cent of high-risk neuroblastoma patients.
Scientists consider people whose cancer has ATRX mutations to represent a specific subgroup of high-risk patients. This is because these alterations never occur alongside amplification of the MYCN gene, which affects about 35 per cent of high-risk patients.
It is not yet known whether neuroblastoma with ATRX mutations is more or less likely than other forms of the disease to respond to immunotherapy. This knowledge gap is limiting scientists’ ability to develop new targeted therapies specific to this patient subgroup.
Making headway in the search for answers
The motivation behind the current study was to try to explain, at least in part, why patients with ATRX-mutated tumours seem destined to face a slowly progressive, treatment-resistant disease course that ultimately results in a poor outcome.
To do this, the team used multiple investigative techniques, working with mouse models, cell lines with different types of ATRX mutations, sequencing datasets and patient samples.
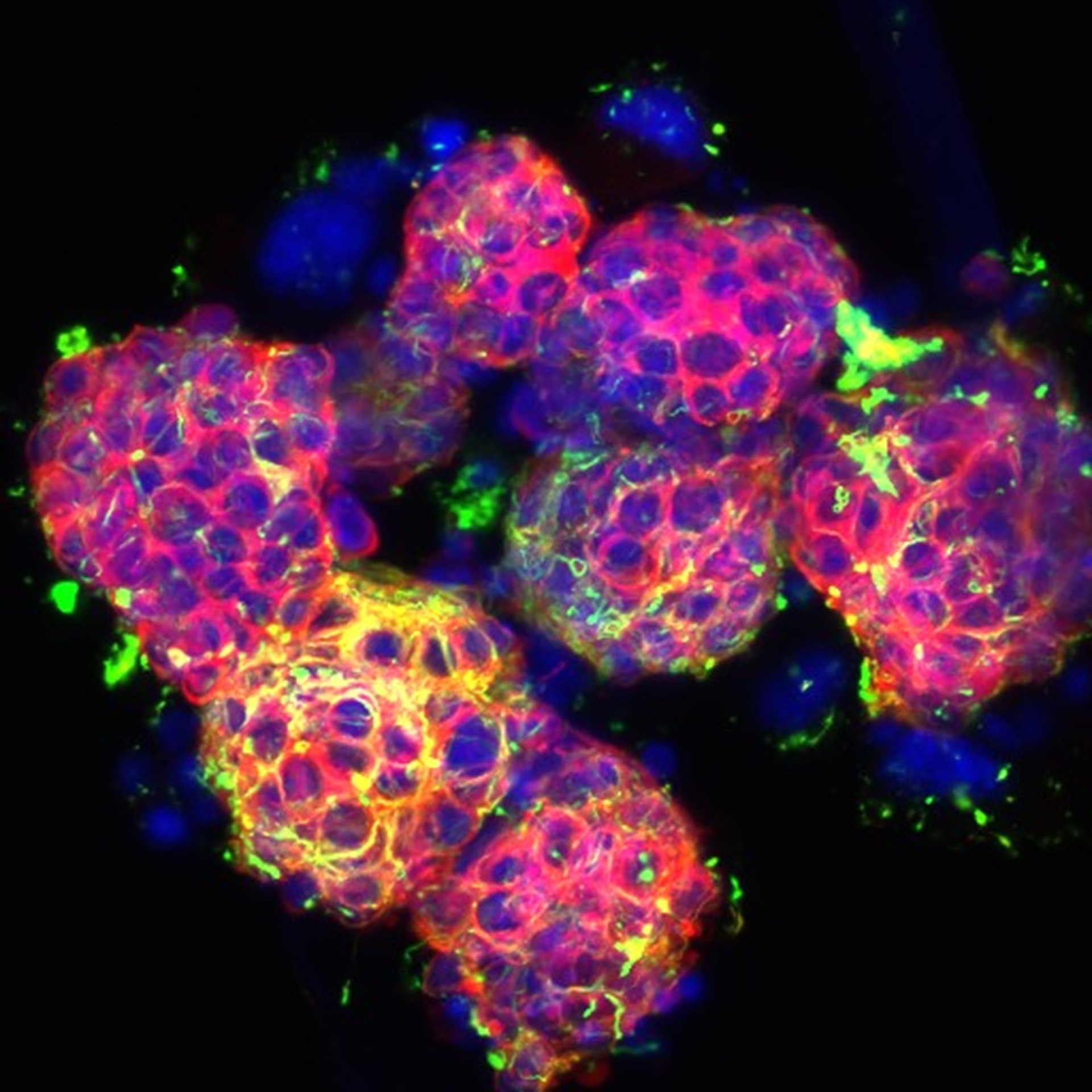
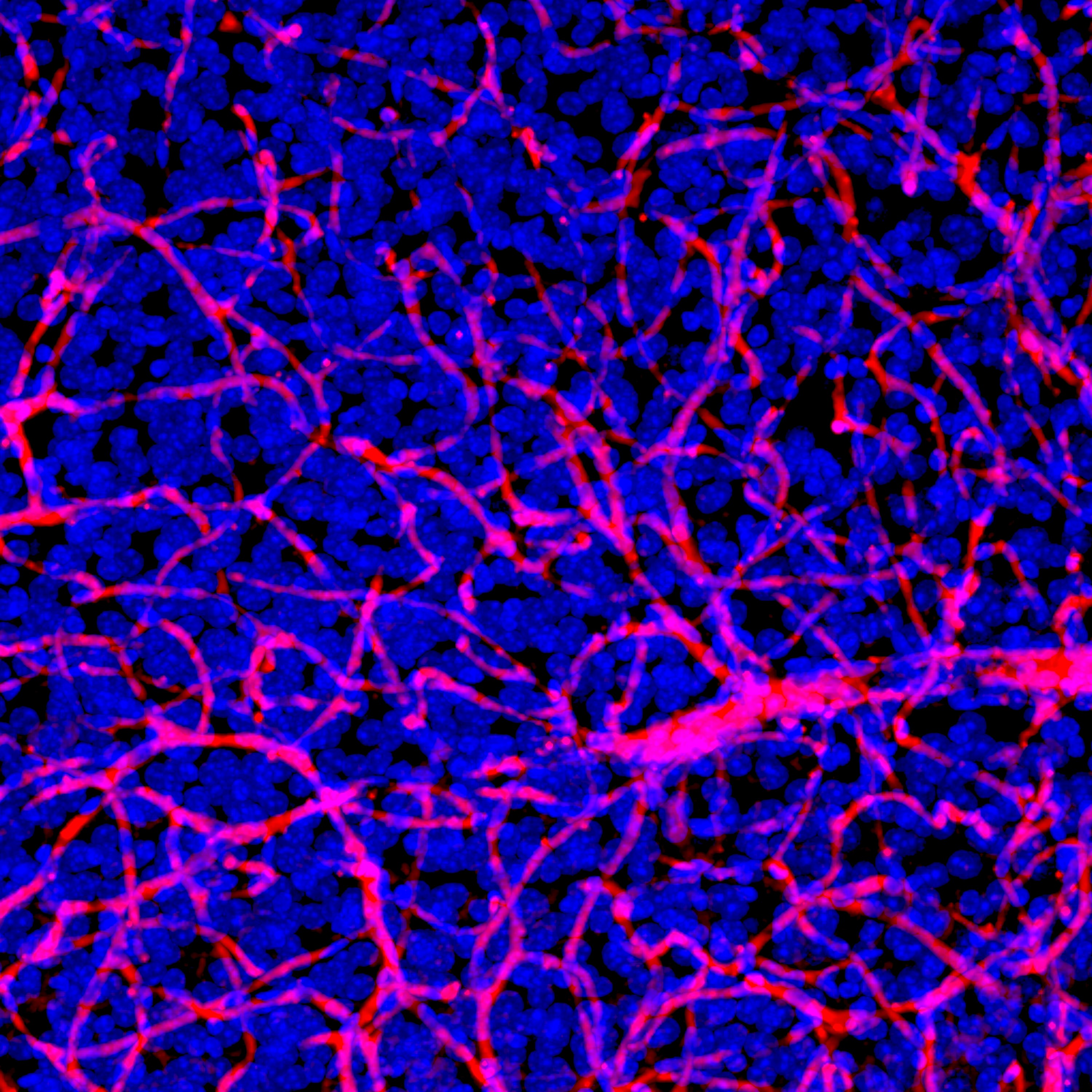
Through a series of experiments, they were able to show that mutations in the ATRX gene lead to the activation of inflammation pathways, which, in turn, increases the recruitment of macrophages into the tumour. Macrophages are a type of immune cell that can, once part of the TIME, promote the survival of cancerous cells, thereby supporting tumour growth.
The scientists demonstrated that the level of immune cell infiltration in tumour samples with ATRX alterations was much higher than that in other subtypes of neuroblastoma, suggesting this may have a role in influencing responses to treatment.
The next stage is to determine whether these genetic alterations are associated with a response to the immunotherapy currently used as standard of care in children with neuroblastoma. If there is a clear link, clinicians could use ATRX status to determine the likely clinical response to this therapy.
“With each experiment, our findings were confirmed”
First author Federica Lorenzi, a Postdoctoral Training Fellow at The Institute of Cancer Research (ICR), said:
“When we first saw the immune changes, we were very surprised and knew we needed to validate this finding in more research models. However, ATRX mutations are only found in one in 10 patients with neuroblastoma, which is a rare disease in itself, so we had few models to work with and very limited data about this subgroup of patients.
“It took us a long time to make new models and to find patient samples and datasets that would help us validate our findings. But with each experiment in a different model, our findings were confirmed.
“One of the challenges we now face is that we need better models of how neuroblastoma cells and immune cells interact. We are working on that as a priority to support further, vital research in this area.”
Senior author Dr Sally George, Group Leader of the Developmental Oncology Group at the ICR and Honorary Consultant Paediatric Oncologist at The Royal Marsden NHS Foundation Trust, said:
“We are delighted to have furthered our understanding of this particular type of high-risk neuroblastoma. More research is needed to translate these findings into a better understanding of how differences in the TIME relate to response to immunotherapy and other agents, but we hope that this insight will contribute to improving outcomes in the future.
“Despite being the most common paediatric solid tumour outside of the brain, neuroblastoma remains challenging to treat in many cases. We are committed to working towards being able to offer each patient targeted treatment based on the genetics of their cancer, which we believe would save many children’s lives each year.”