Timeline: How the ICR has led the way in leukaemia research
For decades, The Institute of Cancer Research (ICR) has been at the forefront of leukaemia drug discovery and development, with our researchers conducting groundbreaking studies and clinical trials to combat this blood cancer.
1960s
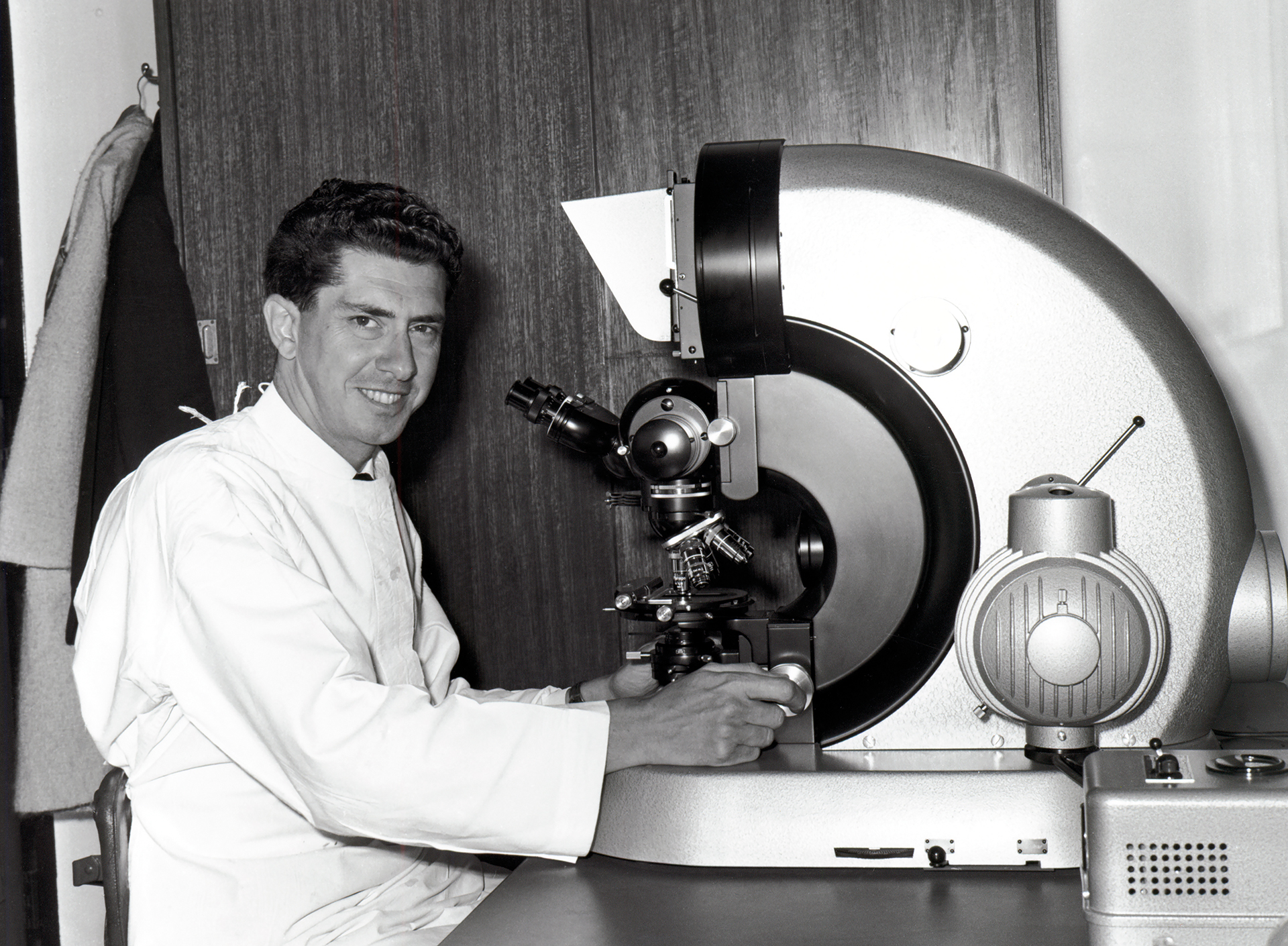
In the early 1960s, Professor Jacques Miller was working as a PhD student at the ICR. Through researching leukaemia in mice, he discovered the essential role of the thymus – where lymphocytic cells mature – in the immune system. This discovery was crucial for understanding how T cells develop, which has significantly advanced leukaemia research and treatment. The findings were published in The Lancet.
1980s
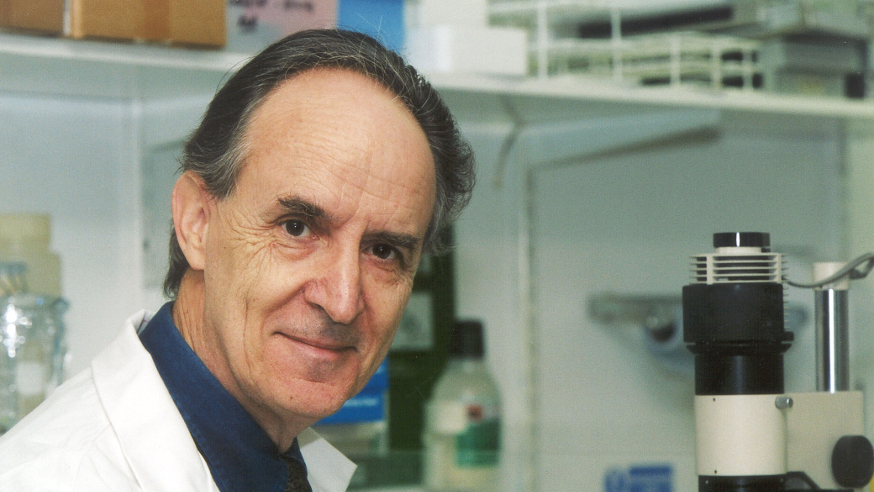
- In 1984, Professor Sir Mel Greaves joined the ICR to establish the Leukaemia Research Fund Centre for Cell and Molecular Biology of Leukaemia.
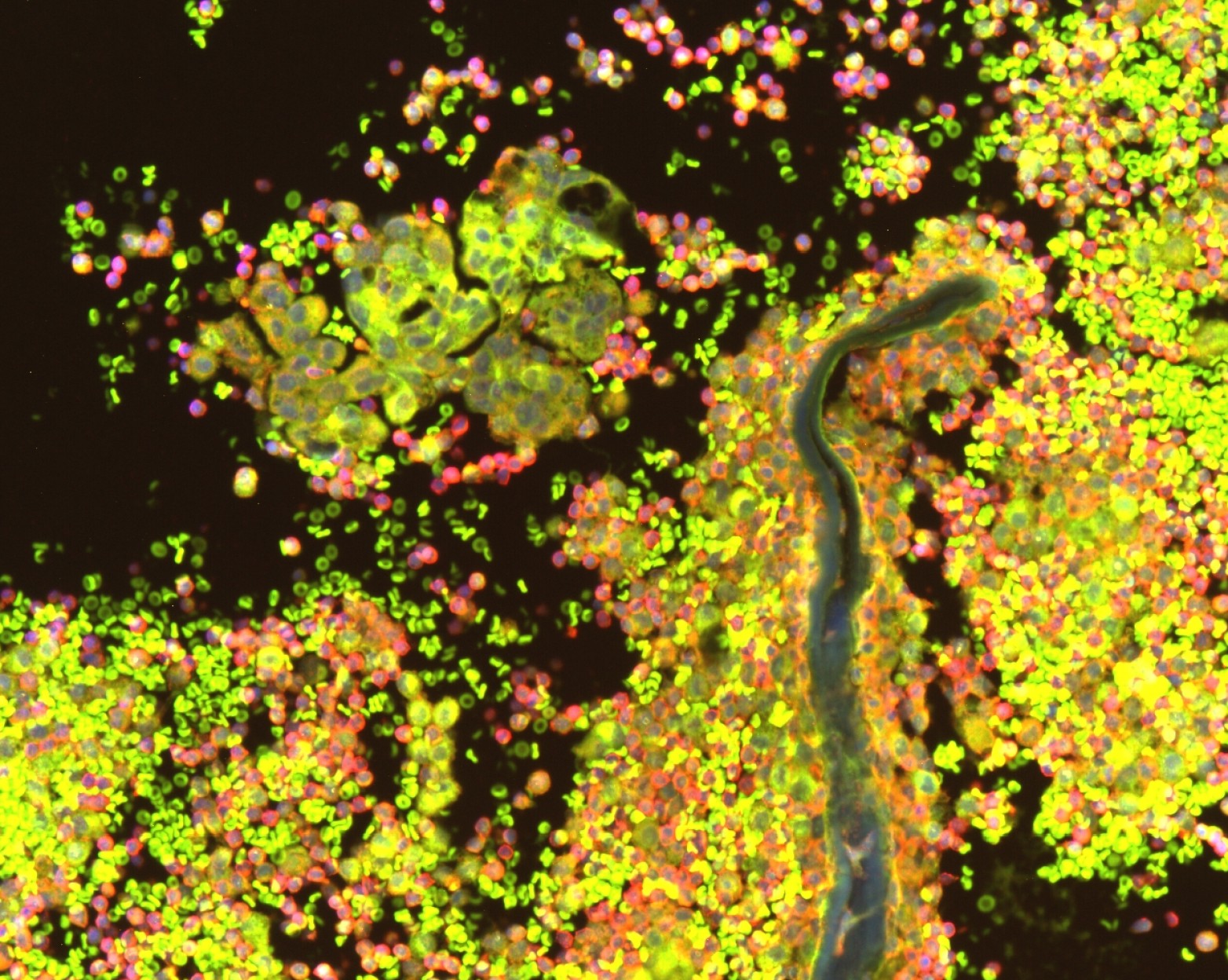
- In 1988, Professor Greaves developed evidence to support the idea that common infections can trigger acute lymphoblastic leukaemia, but only in children who carry a silent pre-leukaemia condition from birth and who had a deficit of immune microbial exposure during infancy. Epidemiological data suggests that the latter exposures derive primarily from the gut microbiome, which formed the basis of Professor Greaves' team's modelling studies in mice.

1990s
- In 1992, the United Kingdom Childhood Cancer Study (UKCCS) – one of the most comprehensive investigations into the causes of childhood cancers, including leukaemia – was initiated. ICR researchers played a pivotal part in the study as one of the key research centres responsible for data collection and analysis.
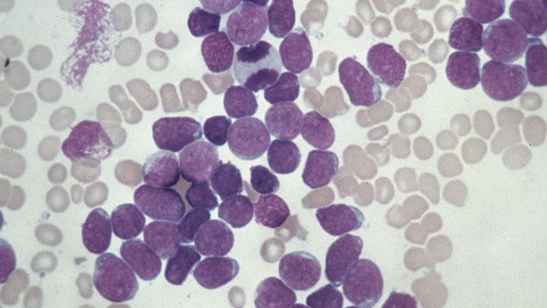
- By 1998, Professor Daniel Catovsky, had initiated three randomised trials into chronic lymphocytic leukaemia (CLL) treatments, which were followed by the Leukaemia Research Fund CLL4 trial in 1999. These early trials provided critical insights into the effective use of chlorambucil in CLL therapy (the main chemotherapy agent), helping Professor Catovsky, and the ICR, refine its dosing and administration to enhance its therapeutic efficacy.
- In the 1990s and early 2000s, various research projects allowed Professor Greaves and his team to identify how and when mutations that can lead to childhood leukaemia occur in the womb, which is where most cases originate.
2000s
- In 2000, ICR researchers led by Professor Sir Mel Greaves discovered that a non-inherited gene abnormality commonly found in childhood leukaemia is present in one per cent of healthy newborn babies. One in a hundred of these babies would go on to develop leukaemia, proving that not every child carrying this genetic abnormality will develop the disease.
- In 2003, as part of the UKCCS, the same team discovered a link between folic acid and leukaemia in children. The research suggested that children exposed to higher levels of folic acid while in the womb have a significantly lower risk of developing leukaemia. Professor Sir Mel Greaves’ work went on to identify possible postnatal triggers that may force blood cells to become leukaemic.
- In 2005, findings from the UKCCS, published in the BMJ, provided significant insights into the development of childhood leukaemia, suggesting that delayed exposure to common infections could trigger the disease in genetically predisposed children.
- A 2007 study, carried out by the ICR and published in Cancer Cell, provided key insights into the complex molecular events that cause acute promyelocytic leukaemia (APL) – a deadly type of leukaemia – and identified potential avenues for therapeutic targeting.
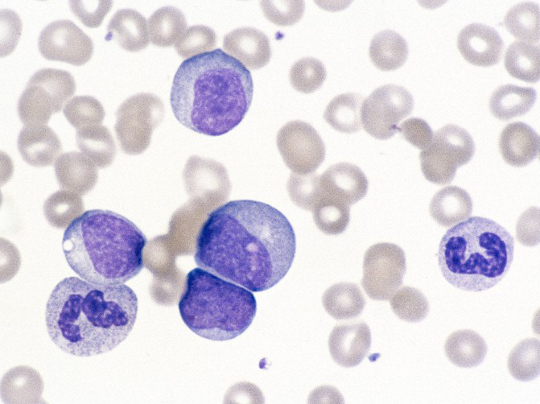
- In 2008, a breakthrough study of identical twins, co-authored by Professor Greaves, provided the first direct confirmation that cancer stem cells cause acute lymphoblastic leukaemia. This discovery, published in the journal Science, strengthened evidence that childhood leukaemia begins before birth.
- In 2008, Professor Richard Houlston led studies revealing that individuals with a close family member affected by CLL have a higher likelihood of being diagnosed themselves. This research, published in Nature Genetics, paved the way for genetic testing and early interventions to help identify those at increased risk.
- In 2009, ICR researchers discovered inherited genetic variants that increase the risk of children developing ALL. The research was published in Nature Genetics.
.jpg?sfvrsn=21a64ae3_1)
2010s
- In 2010, a study led by Professor Houlston uncovered the location of 10 genetic variants, common in the European population, that are associated with an increased risk of CLL. This discovery provided the first evidence that genetic makeup plays a major role in the risk of ALL and insight into how the disease develops. The results were published in Nature Genetics.
- In 2011, ICR researchers found that a genetic test could be used to identify patients with the most common type of adult leukaemia, CLL, who at the time did not respond well to available drugs and should be considered for experimental treatments instead. The research was published in the Journal of Clinical Oncology.
- In 2011, Cancer Research UK-funded researchers at the ICR, led by Professor Richard Marais, revealed a technique to kill chronic myeloid leukaemia (CML) cells that had stopped responding to imatinib – a targeted drug. They showed that a combination treatment consisting of nilotinib, and drugs called MEK inhibitors, destroyed CML cells by blocking a strong molecular survival signal keeping them alive. The research was published in Cancer Cell.
- In 2013, a study led by Professor Houlston, which was published in Blood, identified a heritable gene variant associated with an increased risk of developing CLL.
- In 2013, Professor Greaves and Professor Houlston led groundbreaking genetic studies that deepened our understanding of leukaemia. One study, published in PNAS, sequenced the entire genomes of identical twins with leukaemia, identifying both previously known and newly acquired mutations driving the disease. In the same year, Professor Houlston’s research, published in Nature Genetics, uncovered four new genomic regions linked to increased susceptibility to developing CLL.
- In 2013, Professor Greaves’s pioneering work on cancer resistance and mutations led to a more broader understanding into the role of evolution in cancer development, leading to the establishment of the Centre for Evolution and Cancer at the ICR.
- In 2015, Professor Greaves continued his studies on leukaemia in identical twins and traced the disease’s earliest genetic changes back to immature immune cells that develop before birth. The research was published in Leukemia.
- In 2016, Dr Spiros Linardopoulos discovered a new drug, later named EP0042, that could help counteract drug resistance in cancers such as acute myeloid leukaemia (AML). The drug works by targeting key proteins involved in cancer growth.
- In 2016, an international study co-led by Professor Houlston linked the increased risk of developing CLL to the inheritance of nine separate regions of DNA, each containing genetic variants associated with the disease. The research was published in Nature Communications.
- In 2017, research led by Professor Houlston found that when a specific region of DNA has certain genetic changes, is linked to an increased risk of high-hypodiploid ALL – the most common genetic subtype of ALL, which is associated with good outcomes. Published in Nature Communications, the research points to a likely biological process or event at the cellular level behind the development of the childhood cancer.
- In 2017, Professor Greaves was awarded the Royal Society’s prestigious Royal Medal in recognition of his research on childhood leukaemia.
- In 2018, research led by Professor Houlston and published in Nature Communications identified that two single-letter changes to DNA are linked to an increased risk of developing ALL.
- In 2018, Professor Greaves received a Knighthood for his work advancing the diagnosis, treatment and prevention of childhood leukaemia.
2020s
- In 2021, Professor Greaves wrote a perspective piece in Leukemia, titled “Can we prevent childhood leukaemia?” where he discussed how the rare nature of these cancers meant there was reluctance from industry to invest in drug development. The piece was based on research using mouse models to study how the gut microbiome and infections influence the development of leukaemia, highlighting the environmental factors involved.
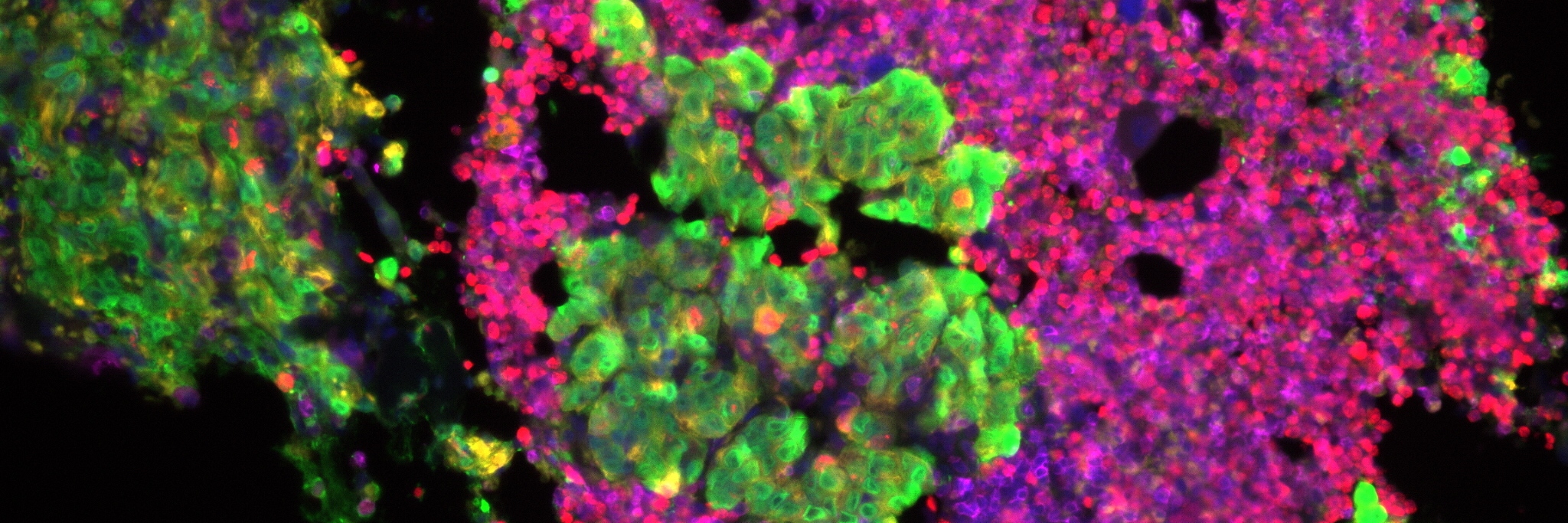
- In 2021, research co-led by the ICR and University College London showed that leukaemic cells can ‘go to sleep’, thereby avoiding the effects of chemotherapy. This breakthrough, published in Nature Cancer, could help direct researchers towards new, more effective treatments that stop the cancer from returning.
- In 2021, Professor Catovsky found that ‘death from infection’ – the leading cause of death for patients with CLL due to their weakened immune systems – is linked to specific genetic mutations. Published in Leukemia, the study showed that testing for these mutations could help identify patients at a higher risk of dying from infection and inform disease management strategies.
- In 2022, a first-of-its-kind twin study following seven sets of twins with ‘discordant’ ALL (where only one twin in each pair, at least initially, had the disease) for 15 years was led by Professor Greaves and published in Leukemia. The study confirmed that leukaemia starts in the womb and could help guide screening when only one twin is affected. These findings will help clinicians advise parents of twins with ALL, offering guidance on risk level and screening.

- In 2023, The US Food and Drug Administration (FDA) granted Orphan Drug Designation (ODD) to EP0042 for patients with AML.
- In 2024, Dr David Taussig led a phase I trial of the ICR-founded drug, EP0042, in collaboration with Ellipses Pharma – which rapidly progressed the development of the drug following successful negotiations led by the ICR’s Business Innovation Office. The clinical trial data was presented at the 66th American Society of Haematology Annual Meeting and published in Blood.
- In 2024, research co-led by Professor Kamil Kranc and the University of Oxford uncovered a promising treatment strategy for AML by targeting the enzymes that AML cells typically use to sense and adapt to changing oxygen levels. The research, published in Nature Cancer, revealed that blocking these oxygen-sensing enzymes can significantly halt AML in mice and in patient samples without affecting the normal production of blood cells.
- In 2024, Dr Alex Radzisheuskaya and Professor Kristian Helin identified a key weakness in AML by focusing on disrupting the function of a protein complex that cancer cells, including leukaemia cells, rely on to maintain their abnormal growth. The research, published in The EMBO Journal, offers a promising strategy to delay the progression of the aggressive cancer.
Your support helps

“When I was diagnosed with leukaemia, I never thought I would still be here.”
Karin Manchester, 65, (pictured) was told she had a week to live after being diagnosed with acute myeloid leukaemia (AML) in 2004. Thanks to treatment and a clinical trial, she has been in remission for 20 years.