Cancer cells can become resistant to treatment – it is one of the main reasons treatments, which were successful to start, can then begin to fail. There are different reasons this can happen and Professor James O’Connor, Professor of Quantitative Biomedical Imaging at The Institute of Cancer Research has a particular interest in one of them: hypoxia.
Hypoxia occurs where the cancer cells in a tumour do not receive enough oxygen. When a tumour grows quickly, it can start consuming more oxygen than the blood vessels near it can supply. This leads to some of the cells in the tumour having lower oxygen levels than they need, which in turn can have an effect on how the cells function.
It forces the cell to adapt to survive and can lead to the tumour becoming resistant to various treatments such as radiotherapy, chemotherapy and immunotherapy. To date, there are no tests that are used in routine clinical practice that can detect or track tumour hypoxia.
Measuring hypoxia
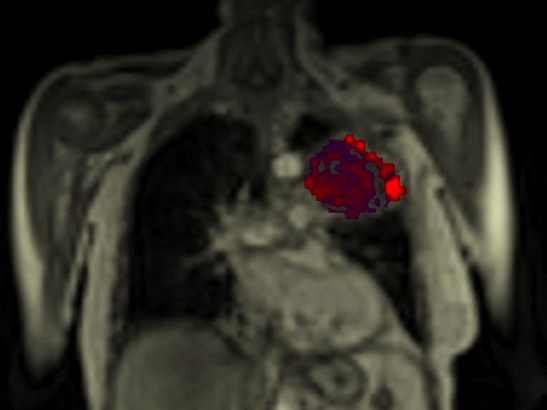
Professor O’Connor is a clinician scientist – alongside his research, he is a practising consultant radiologist. One aspect of his work, which he started in Manchester and is now continuing at the ICR, focuses on finding a way to measure tumour hypoxia in patients. In a recent study, Professor O’Connor and team showed that they could identify, map and quantify hypoxia using a new MRI technique – first in mice and then in patients with lung cancer.
To achieve this, the scientists get patients to breathe air followed by pure oxygen gas. Healthy, well oxygenated tissues see a build-up of free oxygen molecules and this can be detected by MRI, which is why this technique is called ‘oxygen-enhanced MRI’.
However, when extra oxygen is delivered to hypoxic tumour it binds to haemoglobin molecules and so there are no free oxygen molecules to alter the MRI signal.
The scans developed by Professor O’Connor and his team can measure and map the parts of each tumour that behave like well oxygenated tissue and distinguish them from regions that are hypoxic.
This method has the potential to identify patients who have hypoxic tumours and may be resistant to treatment. With this information, patients could be given treatment options that are better suited for them. Having a detailed image of where hypoxic tumour tissue is located could also serve as a map to deliver treatments that target hypoxia and hence improve treatment outcome.
Hypoxia plays a particular role in lung cancer, which is why Professor O’Connor and his team focused on it first – but they are now taking this research forward in other tumour types.
Bench to bedside
This new technique is promising and a great result of combining preclinical animal research and clinical science. James O’Connor’s research group is comprised of people from a range of disciplines, from maths, computer science and physics to clinical medics.
While it can be challenging to coordinate a group with such diverse backgrounds, bringing together experts that might normally be kept apart has its advantages.
“Having clinical experience helps you frame your research questions,” he explains.
Often experiments in the lab are carried out separately from clinical practice.
In Professor O’Connor’s lab, the methods used for the experiments can be carefully chosen from the start to make sure the results found are replicable across both contexts. Translating ideas from the lab into the clinic within one team allows patients to benefit from research quicker.
‘Unlocking potential’
Professor O’Connor also has an interest in improving the information we get from imaging techniques already used in the clinic. “Can we use imaging to predict and monitor response, rather than just locate tumours and measure how big they are?” he asks.
By performing more advanced image analysis, Professor O’Connor believes we could get far more out of the images we’re already taking in the clinic.
“We need to avoid our progress from being just incremental. Data science has great potential, but it's all about unlocking that potential and finding the application that is going to really make a difference for patients.”
This challenge, alongside his ongoing work on hypoxia, is what Professor O’Connor and his team will continue to focus on in the next few years.