Researchers have shown that subtle mutational differences in a gene called ATRX help explain why children with the same type of neuroblastoma respond differently to treatment. These findings could support precise therapy recommendations based on a stronger understanding of the disease’s underlying biology.
Researchers at The Institute of Cancer Research, London, led a team investigating how differences in the exact location of the ATRX mutation can influence how neuroblastoma behaves and responds to treatment.
The study, published in Neoplasia and predominantly funded by a Cancer Research UK Clinician Scientist Fellowship, progresses our biological understanding of neuroblastoma and builds upon growing evidence that ATRX-mutant tumours represent a distinct clinical subgroup of patients. The work was supported by Siobhan's Superstar Legacy, in collaboration with Arcobaleno Cancer Trust. It also adds important detail helping to illustrate the variation seen in patient responses to treatment.
Looking beyond a single genetic label
Neuroblastoma is a childhood cancer that develops in immature nerve cells called neuroblasts, most commonly in the adrenal glands above the kidneys. The presentation of the disease, which typically affects children under five, can vary from slow-growing tumours to aggressive forms that are difficult to treat.
Neuroblastoma is currently treated with a type of differentiation therapy – where drugs induce immature, rapidly-dividing cancer cells to mature into normal, functioning cells. However, increasing evidence suggests that the disease consists of distinct molecular subgroups shaped by genetic and environmental factors, which may respond differently to treatment.
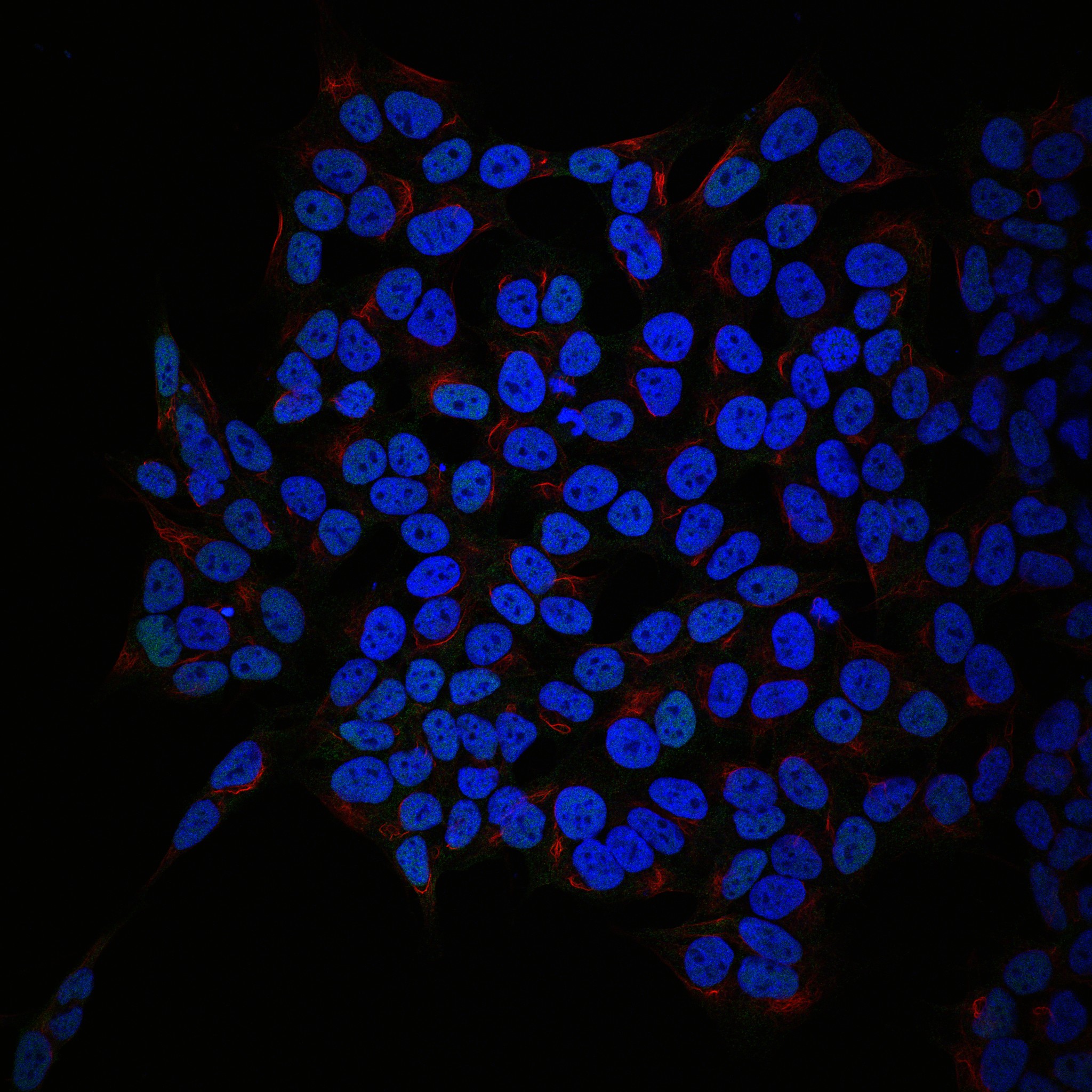
One gene often altered in neuroblastoma is ATRX, which plays an important role in organising and maintaining DNA within cells. Mutations in ATRX are already linked to recognisable patterns in how the disease develops, but children whose tumours carry these mutations can have different responses to treatment.
Until now it has been unclear why this heterogeneity exists. In the study, the research team used stem cell-based laboratory models that replicate disease progression to analyse how various ATRX mutations affect tumour biology. This revealed that alterations in different regions of the ATRX gene are linked to distinct biological behaviours, helping to explain why tumours that appear genetically similar may not respond to treatment in the same way.
By comparing specific ATRX mutations against differences in the tumour’s behaviour and response to treatment, the study helps bridge the gap between fundamental biology and how children with neuroblastoma should be treated in the clinic.
The team’s findings highlight the importance of moving beyond simple mutation categories and towards a more nuanced view of tumour genetics.
Implications for treatment and future research
First author Dr Federica Lorenzi, Senior Scientific Officer in the Paediatric Solid Tumour Biology and Therapeutics Group at The Institute of Cancer Research (ICR), said: “Although most neuroblastomas share the same ATRX mutations, pinpointing the precise location of the mutation can make a real difference to how it influences response to treatment. This helps explain why children with seemingly similar tumours can have very different outcomes.
“In the longer term, a deeper understanding of the tumour biology could allow us to inform clinicians on precise treatment recommendations, rather than a one-size-fits-all approach.”
A step towards more personalised care
While the therapy given to neuroblastoma patients has evidence of clinical benefit for some children, it is challenging to identify those patients likely to benefit. Future work will continue to use stem cell models to investigate neuroblastoma biology in greater depth. This research builds a clearer understanding of how the location of genetic differences drive tumour behaviour and how this knowledge can guide personalised treatment strategies for children living with this unique cancer.
Senior author Dr Sally George, Group Leader of Developmental Oncology at the ICR, said: “What’s particularly exciting is that our ongoing insights from stem cell modelling are directly relevant to how we treat neuroblastoma. This work helps link fundamental biological understanding to clinical decision-making.
“The ultimate goal is to move towards improved patient stratification based on molecular insights and developing novel approaches for certain patient subgroups. By understanding the tumour in greater detail, we hope to make more informed decisions that give every child the best possible chance of a good outcome.”