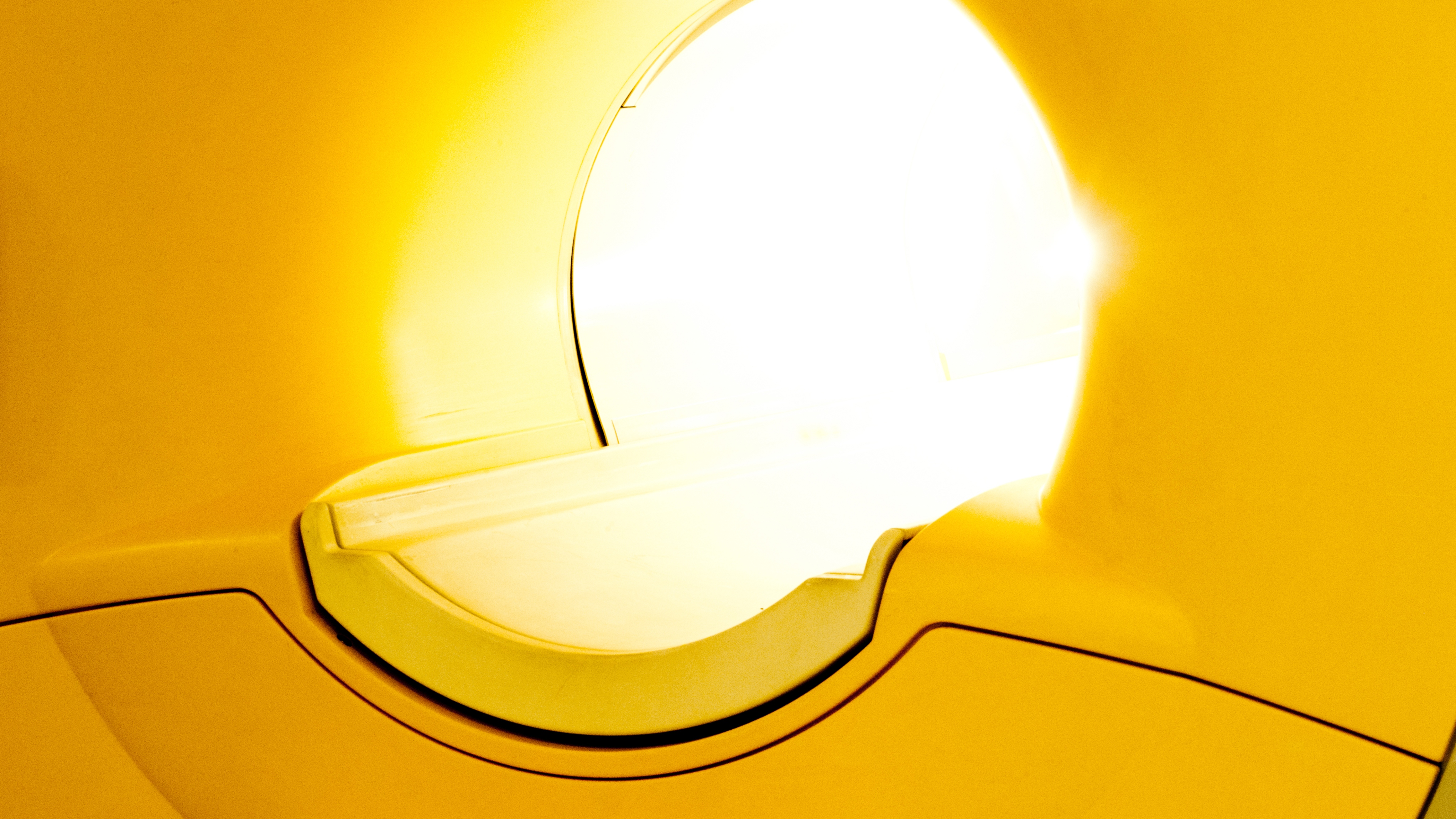
Whole-body MRI scans provide powerful insights into treatment effectiveness and long-term outcomes for patients with myeloma, an incurable but treatable blood cancer.
Results from the iTIMM study led by The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London, have shown that whole-body MRI scans (WB-MRI) can detect tiny traces of the disease, known as minimal residual disease (MRD), in the bone marrow after treatment. This can provide a crucial insight into how well patients with multiple myeloma are responding to treatment and whether they might relapse - offering a potential new standard in how this complex blood cancer is assessed.
The first study to evaluate this technique and predict relapse
The research, published in the Blood Cancer Journal, is the first prospective study to evaluate the prognostic value of whole-body MRI to predict how well myeloma patients respond to treatment, using the international MY-RADS (Myeloma Response Assessment and Diagnosis System) reporting system. MY-RADS is an internationally developed, standardised set of criteria used to interpret and report WB-MRI scans specifically for multiple myeloma. It found that WB-MRI could detect residual disease after treatment, even when traditional blood and bone marrow tests showed no signs of cancer. By predicting relapse, clinicians are able to improve how they tailor a patient’s treatment.
Multiple myeloma is a cancer of the plasma cells, a type of white blood cell responsible for fighting infection by producing antibodies. In myeloma, abnormal plasma cells produce ineffective antibodies, weakening the immune system and increasing vulnerability to infections. While this cancer cannot currently be cured, treatments can effectively control symptoms, extend remission periods, and improve patients’ quality of life.
Patients with residual disease more likely to relapse
Patients with signs of residual disease on post-treatment MRI scans were significantly more likely to relapse and had shorter overall survival. Current response assessments rely on blood tests and bone marrow biopsies, as well as CT scans and X rays. However, these can miss areas of cancer and detect the cancer when it’s too late. WB-MRI offers a way to scan the entire body without the use of radiation, picking up signs of remaining disease in both the bones and soft tissues.
The study included 70 patients undergoing a stem cell transplant. All were scanned via WB-MRI before and after treatment. The results showed that one in three patients had signs of residual disease on WB-MRI after treatment. These patients had a median progression-free survival of just 24 months, compared to 42 months for patients with no visible disease on WB- MRI imaging. Overall survival was also significantly shorter in those with positive MRI findings.
These outcomes were independent of other response measures, including blood markers and bone marrow minimal residual disease (MRD) testing. As imaging continues to advance, it will play an increasingly central role in how clinicians monitor cancer and deliver personalised treatment.
'This study gives us valuable information on how well myeloma has responded to treatment'
Professor Christina Messiou, Consultant Radiologist at The Royal Marsden NHS Foundation Trust and Professor in Imaging for Personalised Oncology at The Institute of Cancer Research, London, and Chief Investigator of the study, said:
“This study shows that whole-body MRI gives us valuable information about how well the myeloma has responded to treatment that other tests may miss. It’s exciting that we now have a standardised, non-invasive imaging method that can be used across cancer centres. WB-MRI doesn’t involve radiation or intravenous injections, which is important for patients who may require lifelong monitoring. This is an important step towards smarter and kinder precision diagnostics for patients with cancer."
Professor Martin Kaiser, Professor of Haematology at The Institute of Cancer Research, London, and Consultant Haematologist at The Royal Marsden NHS Foundation Trust, said:
“Access to this gold-standard precision imaging with whole body-MRI has revolutionised care for myeloma patients. As the treatment options for myeloma increase and factors such as disease distribution across the body are increasingly understood as important to treatment response, the relevance of the whole body-MRI for personalising treatment will only increase over time.”
'This cutting edge treatment not only extended my life but allowed me to continue serving my country'
Air Vice-Marshal (Ret'd) Fin Monahan, Chief Fire Officer South Wales Fire and Rescue Service and patient at The Royal Marsden, was diagnosed with myeloma in 2009 whilst serving in the RAF. He has since relapsed twice, but thanks to whole body MRI scans, his cancer was detected much earlier than would have been possible with a traditional CT scan.
He said: “With the constant threat of relapse, myeloma patients are in a long term mental battle with this insidious disease. However, being part of the whole body MRI scan study at The Royal Marsden allowed my cancer to be closely watched and resulted in me being treated sooner than I would have been under normal protocols.
"This not only extended my life but after diagnosis, I returned to flying jets and to active operational duties. I would eventually not be allowed to fly on medical grounds due to myeloma but paved the way to establishing the first training programme of Ukrainian forces in 2015 and I was called upon to run NATO air operations after the invasion of Ukraine. This cutting edge treatment not only extended my life but allowed me to continue serving my country."
The study was supported by the NIHR Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research, London, The Royal Marsden Cancer Charity, and the Cancer Research UK National Cancer Imaging Translational Accelerator (NCITA).