CLOSED: Targeting Urea Cycle Dysregulation as a Tumour Specific Vulnerability in Lethal Prostate Cancer
Application closing date: 16/11/25
Project background
1 in 5 people with prostate cancer are diagnosed after their cancer has spread beyond the prostate, making the chance of cure low. Despite improvements in the treatment of advanced prostate cancer, all patients eventually develop resistance to approved therapies. This stage of prostate cancer, termed metastatic castration-resistance prostate cancer (mCRPC), is invariably fatal, with an average life expectancy of only 12-18 months. Consequently, prostate cancer remains a leading cause of cancer-related death worldwide [1], highlighting a critical unmet need for new treatment strategies.
A major challenge in developing effective anticancer therapies is targeting cancer-specific vulnerabilities that kill cancer cells without damaging normal tissues, thereby minimizing side-effects. Central to this goal is identifying molecular characteristics unique to cancer cells. One such distinguishing feature is that cancer cells often exhibit distinct cellular metabolism, with metabolic reprogramming being a hallmark of tumorigenesis [2]. This enables cancer cells to adapt, resist treatment, and survive.
Recent advances have highlighted the dependence of mCRPC on amino acid (AA) metabolism, with tumour cells becoming “addicted” to AAs such as glutamine, methionine, and arginine, which support tumour growth and treatment resistance [3-5]. AA metabolism provides essential nitrogen and carbon precursors for energy production, DNA synthesis, and immune cell function, but also generates toxic ammonia, which is cleared through the urea cycle (UC). This makes the UC critical for survival in tumours with high AA metabolism.
While UC dysregulation (UCD) associates with worse prognosis across several cancers [6], its impact in mCRPC remains poorly understood. There is now an urgent need to define the biological and clinical significance of UCD in mCRPC and develop strategies to leverage this metabolic dependency as a therapeutic vulnerability.
Project aims
- Determine the incidence, molecular phenotype, and lineage-specificity of prostate cancer cells characterised by UCD, and define the clinical significance of this prostate cancer subtype
- Elucidate the impact of urea cycle enzyme modulation on prostate cancer cell proliferation, molecular signalling pathways, and endocrine therapy resistance, to identify novel therapeutic targets that exploit urea cycle dysregulation as a cancer-specific vulnerability in mCRPC
- Evaluate the impact of UC abrogation on DNA damage repair and immune cell activation to inform the development of rational drug combinations for the treatment of mCRPC
Further details & requirements
Aim 1: RNA-sequencing (RNA-seq) data from clinical biopsies obtained at diagnosis of castration-sensitive prostate cancer (CSPC), at progression to mCRPC, and from normal non-malignant prostate tissue, will be analysed to identify UC-related genes that are significantly differentially expressed in mCRPC. These gene expression profiles will then be integrated with curated, publicly available UC pathway signatures and metabolic modelling algorithms, to stratify mCRPC samples into high- and low-UC activity subgroups. These subgroups will then be further interrogated to identify genes that are significantly up- or downregulated in mCRPC tumours with elevated UC activity, which may either drive UC pathway activation or enable cellular adaptation to withstand increased levels of potentially toxic UC metabolites and by-products. Additionally, complementary metabolic modelling and gene set enrichment analysis (GSEA) will uncover metabolic and molecular signalling pathways that are enriched in high-UC activity tumours, which may contribute to prostate cancer cell survival and proliferation. Associations with targeted next generations sequencing (NGS) data will also be made to assess co-occurrence of UCD with common prostate cancer genomic alterations, identifying biomarkers predictive of elevated UC activity. To further define lineage specificity, spatial transcriptomics and single-nucleus RNA-seq data from mCRPC biopsies will be leveraged to map the localisation of UC-high prostate cancer cells within the tumour microenvironment and to explore their associations with specific prostate cancer cell populations. To assess the clinical significance of UCD in mCRPC, UC-related gene expression levels and inferred UC activity will be correlated with clinical outcomes, including Gleason score, prostate-specific antigen (PSA) levels, time to CRPC, response to standard of care therapies for CRPC, and overall survival (OS). Identified clinically relevant associations will then be validated in independent, publicly available mCRPC patient cohorts to confirm their prognostic value and potential utility as biomarkers. Taken together, these studies will elucidate the molecular landscape and clinical significance of UCD in lethal prostate cancer.
Aim 2: Baseline UC activity will be established across a panel of prostate cancer cell lines representing distinct disease states, as well as immortalized benign prostatic epithelial cell lines. RNA-seq data from these models will be analysed to determine the expression of key UC-related genes, UC pathway enrichment, and UC activity (metabolic modelling) to stratify models into UC-high and UC-low groups. This classification will be validated using targeted liquid chromatography–mass spectrometry (LC-MS) to measure urea cycle intermediates. Targeted genetic modulation of key UC-related genes will then be performed across these prostate cancer cell lines. Gene knockouts will be generated using CRISPR-Cas9 or siRNA-mediated silencing, while overexpression will be achieved via CRISPR activation or plasmid-based transfection. Target gene knockout/overexpression will be confirmed by qPCR and Western blot, and targeted metabolomics (LC-MS) will be performed to confirm changes in UC intermediates. Parallel experiments in benign prostate epithelial cells will serve as controls to distinguish cancer-specific dependencies. Following UC-gene modulation, changes in cell viability (CellTitreGlo®) and total protein content (Sulforhodamine B assay) will be compared to unmodified controls, to assess the impact on cell growth. Genes that, when knocked down, selectively inhibit cancer cell growth or, when overexpressed, specifically promote cancer cell proliferation, without affecting the growth of benign prostate epithelial cells, will then be further evaluated as candidate therapeutic targets. To elucidate the molecular mechanisms underlying these effects, RNA-seq analyses will be performed on modified prostate cancer cells to identify changes in gene expression and molecular signalling pathways associated with altered UC activity, compared to unmodified controls. Key pathway alterations will then be validated by qPCR and Western blotting to confirm their impact on downstream signalling nodes, followed by functional interrogation through targeted inhibition to assess their potential therapeutic vulnerabilities in UC-high or UC-low prostate cancers. Taken together, these studies will provide mechanistic insights into how UCD influences CRPC biology and identify therapeutic targets to leverage USD as a cancer-specific vulnerability in mCRPC.
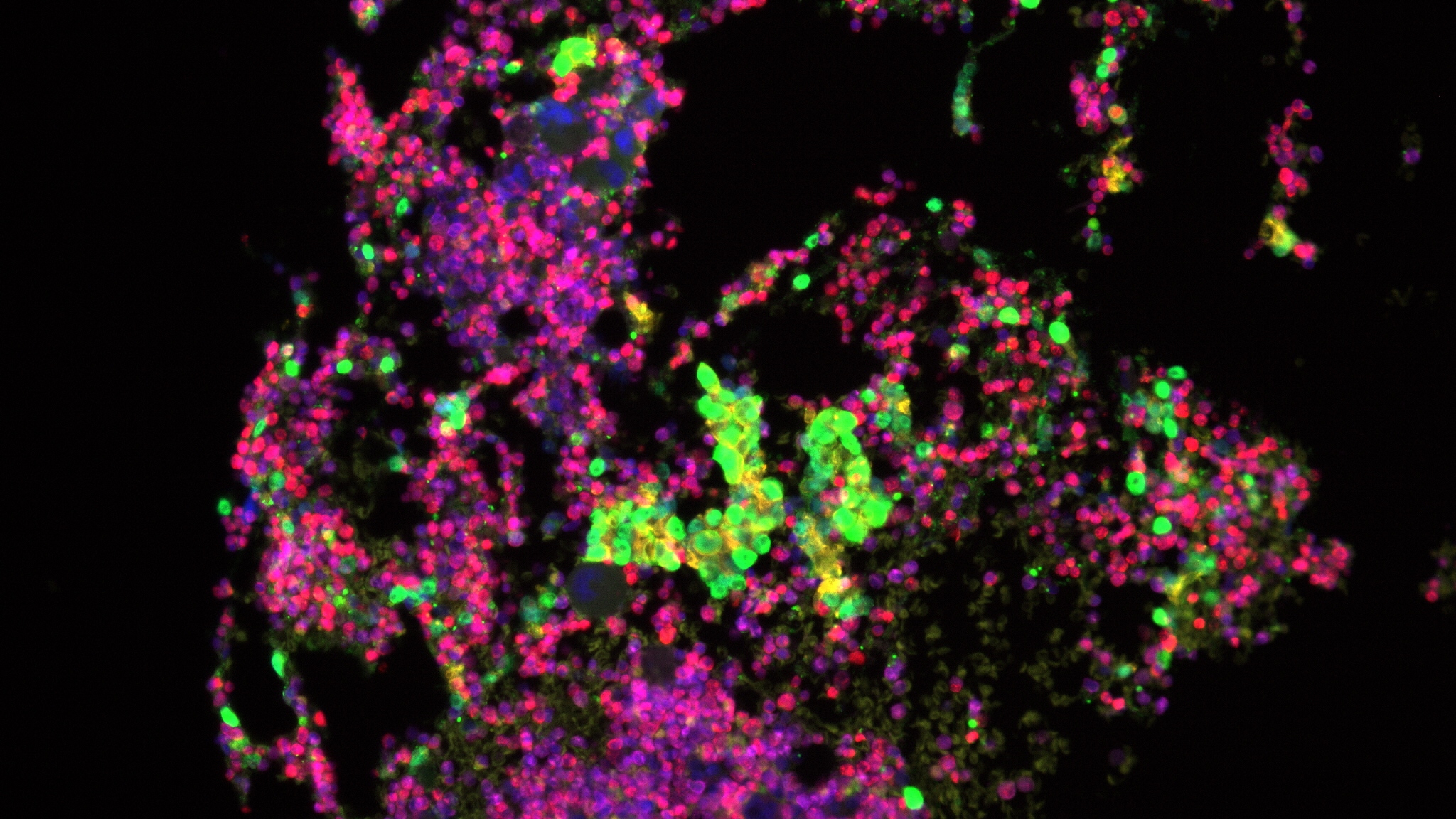
Aim 3: Targeted siRNA knockdown of key UC-related genes will be performed across a panel of prostate cancer cell lines to investigate the functional impact of UC abrogation. To elucidate the mechanisms through which abrogated UC-related genes induced DNA damage, RNA-seq analyses will be performed following target gene knockdown compared to non-targeting siRNA controls and alterations in DNA repair genes and associated signalling pathways determined. Given the role of UC intermediates in pyrimidine biosynthesis, targeted LC-MS/MS will also be performed to quantify intracellular nucleotide pools and assess shifts in the pyrimidine-to-purine ratio. Additionally, BrdU incorporation and DNA fiber assays will be used to evaluate how UC disruption affects DNA replication fork progression and stability. To investigate the impact of UC abrogation on immune cell activation, Western blotting will be performed for markers of immunogenic cell death (ICD) following UC-related gene knockdown. In parallel, RNA-seq data will be analysed to identify changes in immune-related gene expression and pro-inflammatory signalling pathways compared to non-targeting siRNA controls. To functionally assess immune activation, transwell co-culture studies will be conducted following UC-related gene knockdown. Downstream immune effects will then be evaluated by measuring changes in damage-associated molecular patterns (DAMPs), cytokine secretion, immune gene expression, and immune cell activation (flow cytometry). Additionally, rescue experiments will be performed using inhibitors of ICD (Necrostatin-1, Disulfiram). Together, these studies will identify mechanisms through which UCD impacts DNA repair and immune cell activation, informing the rational design of combination therapies for mCRPC.
First or 2:1 in biological or medical sciences or related subject area
1. Sung, H., J. Ferlay, R.L. Siegel, et al., Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians, 2021. 71(3): p. 209-249.
2. Hanahan, D. and R.A. Weinberg, Hallmarks of cancer: the next generation. Cell, 2011. 144(5): p. 646-74.
3. Bidgood, C.L., L.K. Philp, A. Rockstroh, et al., Targeting valine catabolism to inhibit metabolic reprogramming in prostate cancer. Cell Death & Disease, 2024. 15(7): p. 513.
4. Uo, T., C.C. Sprenger, and S.R. Plymate, Androgen Receptor Signaling and Metabolic and Cellular Plasticity During Progression to Castration Resistant Prostate Cancer. Frontiers in Oncology, 2020. Volume 10 - 2020.
5. Yao, P., S. Cao, Z. Zhu, et al., Cellular Signaling of Amino Acid Metabolism in Prostate Cancer. Int J Mol Sci, 2025. 26(2).
6. Lee, J.S., L. Adler, H. Karathia, et al., Urea Cycle Dysregulation Generates Clinically Relevant Genomic and Biochemical Signatures. Cell, 2018. 174(6): p. 1559-1570.e22.