Translational Genetics Group
Professor Clare Turnbull's group is investigating ways to optimise ‘next-generation’ sequencing technologies and analyses of these data in order to identify novel cancer predisposition genes.
Professor Clare Turnbull
Group Leader:
Translational Genetics
Clare Turnbull is a Professor of Translational Cancer Genetics at the ICR. Having trained as a Clinical Geneticist, her clinical work as an NHS Consultant focuses on management of patients and families with hereditary forms of cancer at The Royal Marsden NHS Foundation Trust. Clare has trained in epidemiology and public health, is a fellow of the Faculty of Public Health Medicine and FPH lead for genomics; she has an honorary appointment as a Consultant in Public Health Medicine at the National Disease Registration Service.
Researchers in this group
 .
.
Email: [email protected]
Location: Sutton
Kerstin is currently an Administrative/project Assistant at the Institute of Cancer Research, working within Professor Clare Turnbull’s laboratory in the Division of Genetics and Epidemiology. In this role, my current focus is supporting the BRCA and RETRO projects, where I provide high-level administrative and project coordination support to ensure the smooth delivery of complex research activities.
 .
.
Email: [email protected]
Location: Sutton
Zehra Akar is an Administrative Assistant at the Institute of Cancer Research, within Prof. Clare Turnbull’s team in the Division of Genetics and Epidemiology. With a background in Public Health Policy and Reproductive Health and experience working in academic institutions and diagnostic laboratories, Zehra is currently providing administrative and operational support to the Jewish BRCA Testing Programme.
 .
.
Email: [email protected]
Location: Sutton
Sophie is a Data Manager and part-time PhD student at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. With a background in bioinformatics and genetics, Sophie’s current research focuses on quantifying evidence for variant interpretation in inherited cancers, as well as co-ordinating the CRUK-funded Cancer Gene MAVE (CG-MAVE) grant, and supporting operation of the Cancer Variant Interpretation Group UK (CanVIG-UK).
 .
.
Email: [email protected]
Location: Sutton
Miriam Babigumira is a Research Administrator at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. Having trained academically as a botanist, Miriam’s ethnobotanical work focused on documenting medicinal plant uses, supporting the sustainable use of plant resources, and contributing to community-led research. Her MSc in Women’s Health provided further insight into key areas of interest such as screening, early diagnosis, reproductive risk factors, lifestyle, and environmental exposures. Miriam draws on this training to bring an interdisciplinary approach to working collaboratively across various teams within Institute of Cancer Research and community partners in delivering programme objectives ethically as well as within agreed timeframes. Miriam is currently working on the Jewish BRCA Testing Program.
 .
.
Email: [email protected]
Location: Sutton
Rebekah Beaumont is a Research Administrator at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. Rebekah has contributed to both the NHS Jewish BRCA Testing Programme and the NHS Retrospective Genetic Testing Programme. She completed her master's degree in Genomic Medicine in 2025, co-led by Kings College London and City St George’s University London, where her dissertation focused on variant interpretation in undiagnosed paediatric cases of cerebellar ataxia.
 .
.
Email: [email protected]
Location: Sutton
Nicola Bell is a Genomics Practitioner at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. Nicola is currently working on the NHS Jewish BRCA Testing Programme and the NHS England Retrospective Genetic Testing Programme. Nicola studied Biology at the University of Nottingham, graduating in 2022. Alongside her work at the ICR, she is completing an MSc in Genetic and Genomic Counselling with Cardiff University, due to graduate in 2026.
 .
.
Dr Alice Garrett is an honorary clinical lecturer within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology and a consultant in Cancer Genetics at St George’s Hospital. Having completed her PhD on sarcoma susceptibility at the ICR, Alice currently works on variant interpretation in cancer susceptibility genes with Cancer Variant Interpretation Group UK (CanVIG-UK).
 .
.
Email: [email protected]
Location: Sutton
Charlotte Hennessy is a Research Administrator for the NHS Jewish BRCA Testing Programme. She works within the Genetics and Epidemiology team under Professor Clare Turnbull. She recently transferred from The Royal Marsden Hospital trust where she was working in the Clinical Genetics team.
 .
.
Email: [email protected]
Location: Sutton
Zeid Kuzbari is a bioinformatician with a research focus on NGS whole-exome analyses of testicular germ cell tumours and breast cancer. He is also currently working on the implementation of functional assays of cancer susceptibility genes into the CanVar-UK data platform, supporting variant interpretation. Zeid completed a PhD in Genetics and Epidemiology at the ICR, holds a MSc in Biomedical Science from Université de Montréal, and has a strong background in immunology.
 .
.
Email: [email protected]
Location: Sutton
Sarah Lane is a Scientific Project Manager at the Institute of Cancer Research within Professor Clare Turnbull’s team in the Division of Genetics and Epidemiology. Sarah is a registered associate public health nutritionist with a MSc in Global Public Health and Nutrition, and has previous experience working in policy research funding management, focusing on nutrition, maternal health, and health inequalities funding initiatives. Sarah is currently working on the delivery of the NHSE Retrospective Genetic Testing Programme and Jewish BRCA Testing Programme.
 .
.
Email: [email protected]
Location: Sutton
Dr Lucy Loong is a Cancer Research UK funded Clinical Research Fellow at The Institute of Cancer Research, a partnership analyst at the National Disease Registration Service, and a specialist doctor in Clinical Genetics. Her research focuses on the large-scale integration of nationally collected clinical genetic testing data and rare genetic disease registries with electronic healthcare records, including cancer registry data and hospital episode statistics. Using these linked population-level datasets, she applies data-driven and longitudinal analytic approaches to study cancer risk and outcomes, evaluate clinical service delivery, and assess cancer surveillance in individuals with inherited cancer susceptibility syndromes.
 .
.
Email: [email protected]
Location: Sutton
Yana Moscovitz is a Research Administrator at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. Yana joined the NHS England Retrospective Genetic Testing Programme in 2025 after completing an MSc in Medical Genetics at the University of British Columbia.
 .
.
Email: [email protected]
Location: Sutton
Sudeekshna Muralidharan is a Research Administrator in the Translation Genetics Team under Professor Clare Turnbull at the Institute of Cancer Research. She is a double-MSc graduate with an MSc in Genetics of Human Disease from UCL and an MSc in Cancer, Molecular Pathology and Genomics from QMUL. She completed her BSc (Hons) in Biomedical Sciences at KCL in 2021. She started working on two projects at the ICR in May 2024. She has since been working solely on our largest ongoing programme, JBRCA, which currently tests over 43,000 patients. She is very interested in project management and hopes to develop her career within that discipline. She has an international background and was born in India but raised in Singapore and Belgium. She moved to London in 2018 for higher education and has been living there since.
 .
.
Email: [email protected]
Location: Sutton
Josh is a research Genetic Counsellor within the group, primarily helping to guide patients through their germline genetic testing process, aiding their adjustment journey when we identify pathogenic variants, and facilitating cascade testing for their at-risk relatives. Josh holds Health and Care Professions Council registration as a Clinical Scientist following completion of the NHS Scientist Training Programme in Genomic Counselling in Oxford in 2021. He also has quantitative and qualitative research experience from the University of Oxford studying the return of germline pathogenic variants as secondary findings from the NHS 100,000 Genomes Project.
 .
.
Email: [email protected]
Location: Sutton
Esther is a Research Administrator working within Professor Clare Turnbull’s team in Genetics and Epidemiology at the Institute of Cancer Research. Esther joined the ICR in 2024 to support the delivery of the Jewish BRCA Testing programme, population testing for hereditary cancer risk. With an academic background in Cancer Sciences and interest in public engagement, Esther is keen to develop her skills in both public engagement and clinical trials in oncology.
 .
.
Andrea Osborne is a Research Administrator in the Division of Genetics and Epidemiology at the Institute of Cancer Research, working within Professor Clare Turnbull’s team. She joined the ICR in 2014 after roles in the NHS and Local Authority, initially supporting the Oncogenetics Teams as Data Manager on key prostate cancer studies including UKGPCS, GENPROS and BARCODE1.
 .
.
Email: [email protected]
Charlie is a research bioinformatician within the Translational Genetics team. He completed his PhD at the University of Manchester in 2022, developing approaches for the prioritisation and investigation of splice-impacting variants in Mendelian disease. His current research focuses on developing methodologies to support the integration of functional data, particularly multiplex assays of variant effect (MAVEs), in the interpretation of germline variants in cancer susceptibility genes (CSGs). He also administers the CanVar-UK web platform for CSG variant interpretation.
 .
.
Beth is a Scientific Programme Manager at the Institute of Cancer Research, within Prof Clare Turnbull’s team in the Division of Genetics and Epidemiology. She also has an honorary contract within the Cancer Genetics Unit at the Royal Marsden NHS Foundation Trust and the Wolfson Institute of Population Health at Queen Mary University of London (Prof Ranjit Manchanda).
Professor Clare Turnbull's group have written 212 publications
Most recent new publication 2/2026
See all their publicationsResearch and projects in this group
Our group focuses on molecular, statistical and public-health-related population analyses to better implement cancer susceptibility genetics for risk stratification, cancer early diagnosis and prevention.
The research conducted by Professor Clare Turnbull's group focuses on molecular, statistical and public-health-related population analyses to better implement cancer susceptibility genetics for risk stratification, cancer early diagnosis and prevention. This includes:
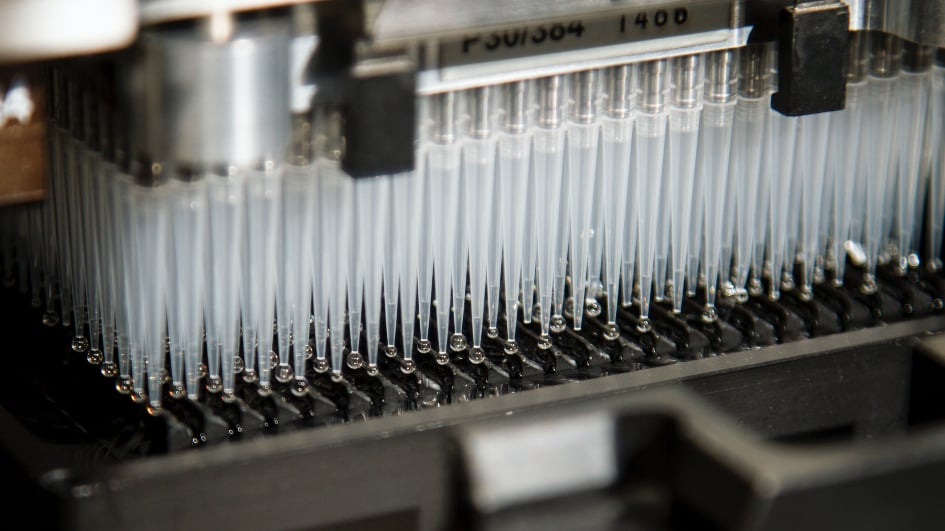
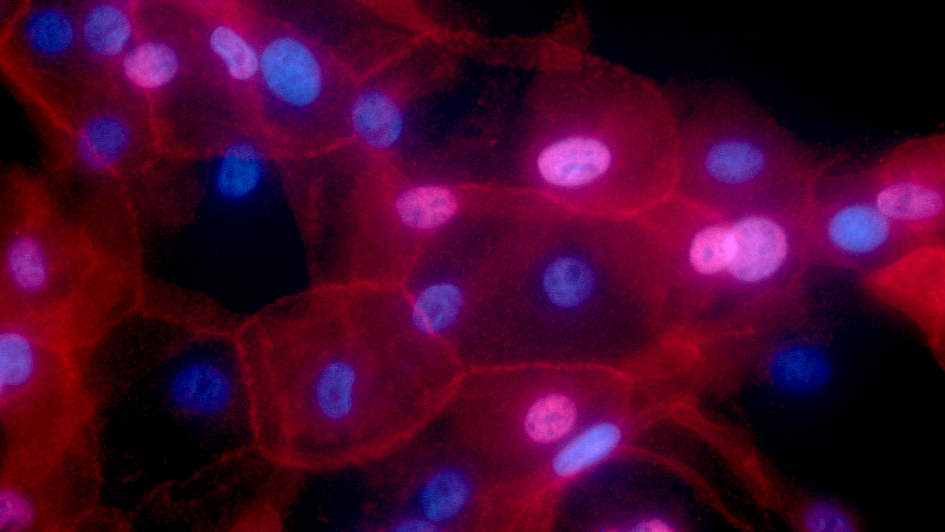
- Laboratory sequencing and genotyping of germline DNA samples from patients with cancer (especially familial types) to identify and understand new (susceptibility, predisposition) genetic factors associated with cancer.
- Clinical interpretation of genetic variants: to understand which of the millions of variants identified on genomic sequencing are pathogenic (disease-associated) and which are benign (innocuous). Clare leads a multicentre CRUK programme award working with David Adams (Sanger) and Greg Findlay (Crick) to explore the role in variant interpretation of MAVEs (Multiplex Assays of Variant Effect). She has since 2017 led CanVIG-UK (Cancer Variant Interpretation Group UK), a group comprising >300 NHS clinical diagnostic scientists, clinical geneticists and genetic counsellors that meets monthly to advance national consensus on clinical variant interpretation for cancer susceptibility genes and maintains the CanVar-UK web resource.
- Instigating routine central submission of NHS data on germline genetic testing to improve clinical practice and inform research. Via the Turnbull-led CRUK-funded CanGene-CanVar Catalyst Programme (2019-2025), the 17 NHS diagnostic labs in England now routinely submit to NDRS individual-level data from all diagnostic genetic testing of cancer susceptibility genes. These data can be linked to cancer registrations and multiple other datasets to understand the national patterns of and outcomes from germline genetic testing for cancer genes.
- Public-health related analyses of the efficacy of genomic approaches to improve cancer early detection (screening) and prevention, including MCED population screening and risk stratification by polygenic risk scores.
- Transforming NHS clinical patient pathways to enable expansion of germline genetic testing: In 2019 we developed the BRCA-DIRECT pathway (digital pre-test information, saliva sampling, genetic counselling telephone helpline, automated laboratory workflows and systematised clinical communication/correspondences), a clinician-lite, patient-centred pathway for mainstream oncology testing for BRCA=gene changes, hypothesising this would enable expansion of testing volumes without incurring increased pressure on the genetics or oncological workforces.
Following our CRUK-funded randomised trial in 1400 breast cancer patients in 5 NHS hospital sites, the pathway has been rolled out as a standard-of-care mainstreaming transformation project in North Thames GMSA (2023-2025, for up to 6000 newly diagnosed breast cancer patients). We have adapted this pathway to enable delivery of The NHS Jewish BRCA Testing Programme (2023-2026) in conjunction with Professor Mike Hubank’s group the RMH Centre for Molecular Pathology.
- Studies of Testicular Germ Cell Tumour Susceptibility
- UK Genetics of Testicular Cancer Study
- Genetics of Multiple Cancers Study
Studies of Testicular Germ Cell Tumour Susceptibility
Testicular germ cell tumour (TGCT) is the most common cancer in men aged 15–45 years and affects nearly 2,000 men in the UK per year. Family history is an important risk factor for the disease. If a man has a brother who has suffered testicular cancer, his risk of developing the disease is 8–10 fold increased compared to a man without any family history of disease. This risk is much higher than the equivalent risks for most other cancer types (typically 2–3 fold elevated). These observations indicate that genes are important in causing testicular cancer.
We have previously identified six genomic regions and more recently an additional nine genomic regions associated with testicular cancer. These, in conjunction with regions identified in international collaborative experiments to which we have contributed, bring the total number of regions identified to eighteen. We aim to identify further regions of the genome associated with testicular cancer and additionally to use new technologies to sequence many thousands of genes in order to identify the genes involved in causing testicular cancer.
UK Genetics of Testicular Cancer Study
MREC: 06/MRE06/41
We are now recruiting all cases of testicular cancer through the UK Genetics of Testicular Cancer Study.
This includes cases of testicular cancer with a family history of the disease and those without a history.
We have recruited 3,000 men to this study and aim to increase this number to 10,000. The blood samples and information from men involved, are used in studies to identify testicular cancer predisposition genes.
Any man who has had testicular cancer and has completed his treatment can participate in this study. Participation in the study simply requires the man to:
1. Provide a blood sample.
2. Complete a short questionnaire about himself and his family.
If you would like more information about the study, download the Patient Information Sheet. If you are interested in participating, contact the study coordinator, Darshna Dudakia, who can provide additional information. Alternatively, phone the research group on 0208 722 4283.
Study Coordinator email: [email protected]
References
Rapley, E.A. et al. A genome-wide association study of testicular germ cell tumor. Nat. Genet. 41, 807-810 (2009)
Turnbull, C. et al. Variants near DMRT1, TERT and ATF7IP are associated with testicular germ cell cancer. Nat. Genet. 42, 604-607 (2010)
Ruark, E. et al. Identification of nine new susceptibility loci for testicular cancer, including variants near DAZL and PRDM14. Nat. Genet. (2013)
Schumacher, F. et al. Testicular germ cell tumor susceptibility associated with the UCK2 locus on chromosome 1q23. Hum Mol Genet (2013)
Chung, C. et al. Meta-analysis identifies four new loci associated with testicular germ cell tumor. Nat. Genet. (2013)
Genetics of Multiple Cancers Study
The aim of the Genetics of Multiple Cancers Study (GeMCaS) is to collect biological samples and clinical data from individuals who have had two or more primary cancers. This will help us to identify, and better understand, the genetic factors that predispose to the development of multiple tumours. In turn, this will facilitate diagnosis and risk evaluation and will enable the development of guidelines for management of individuals and families at increased risk of developing cancer.
Study coordinator email: [email protected]
Current vacancies in this group
There are currently no vacancies available in this group or area.
Recent discoveries from this group
).jpg?sfvrsn=83bdab30_1)
Genetic study links common form of testicular cancer to rare variants in cell structure genes
Breast cancer risk model provides reassuring data for those with family history of disease after short-term HRT use

Genetic testing for Lynch Syndrome prevents cancers being missed