As we enter 2026, scientists at The Institute of Cancer Research, London, share the developments expected this year that could soon change how cancer is treated – from technologies designed to deliver drugs directly into tumours, to new ways to harness the immune system. Some are approaching regulatory approval, others are entering clinical trials, but all point to a future of smarter, kinder, cancer treatment.
Harnessing the immune system
Immunotherapy has transformed outcomes in several cancers, but prostate cancer has remained an exception. Traditional immune-based approaches have shown limited benefit, in part because prostate tumours are adept at evading immune detection – they are ‘immune-cold’.
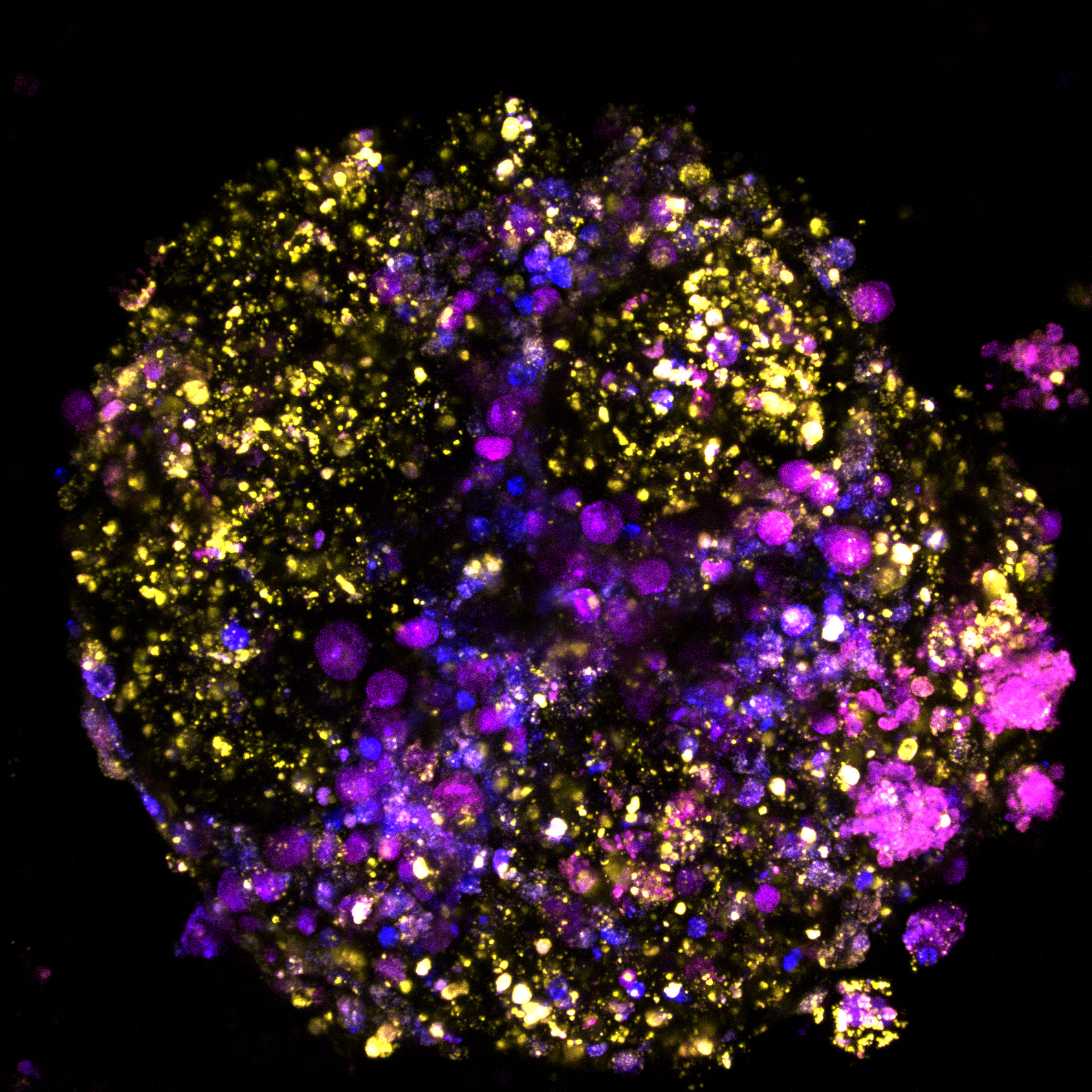
T-cell engagers (TCEs) are a form of antibody designed to link the body’s cancer-killing immune T cells to tumour cells – one half is engineered to latch onto antigens found on the surface of cancer cells, while the other half binds to T cells. By bringing T cells directly to the tumour, TCEs help the immune system to attack the cancer more effectively.
In advanced prostate cancer, TCEs have shown promise in early-stage clinical trials, suggesting these therapies could offer a new treatment option where few exist. ICR researchers are now trialling newer versions of these TCEs, which it is hoped will reduce the need for frequent treatments and hospital visits.
Professor Johann de Bono, Professor of Experimental Cancer Medicine at the ICR, said:
“The future of T-cell engagers in prostate cancer treatment is really exciting, with much expected in the next year or two. As we see research progress, these therapies could move into earlier stages of prostate cancer, potentially increasing cure rates and transforming the way prostate cancer is treated.”
From inhibition to elimination and permanent inactivation
Historically, most drugs to treat cancer have focussed on blocking the activity of a specific, cancer-causing protein. A key issue with this approach is that drug resistance can occur, through a number of mechanisms, as the problematic protein is still present.
New approaches take drug development a step further. They aim to either eliminate the protein entirely, or to exploit it to kill the cancer cell. One of these methods, RIPTACs (Regulated Induced Proximity TArgeting Chimeras), has trial results expected this year.
Dr Adam Sharp Leader of the Translational Therapeutics Group at the ICR, said:
“There’s a novel approach, called RIPTACs, which sticks together two proteins within a cancer cell. One protein is specific to the cancer cell, meaning that only the cancer cell and not normal cells are affected by the drug, and the second protein is one that is essential for the cancer cell to survive. By inactivating this protein, the RIPTAC forces the cell to die – and specifically only the cancer cell. These are being explored in early phase clinical trials at the ICR, for the treatment of lethal prostate cancer currently.”
Targeted protein degradation (TPD) is another technique to destroy a problematic protein. It harnesses the cell’s own waste disposal system – binding the target protein with one which will mark it for destruction.
The first drug derived from this approach, vepdegestrant, is currently under active review and is widely expected to be approved by FDA for the treatment of patients with advanced breast cancer soon.
The ICR has been one of the pioneers and world-leading academic centres in this field, and the early discoveries in the Centre for Cancer Drug Discovery at the ICR led to the creation of a spinout in 2018, Monte Rosa Therapeutics.
Professor Zoran Rankovic, Director of the Centre for Protein Degradation at the ICR, said:
“Targeted protein degradation is highly innovative and one of the most promising new approaches to emerge in drug discovery research in the past decade, and it is poised to reach a major milestone in 2026, with the expected FDA approval of vepdegestrant.
“One of the programmes developed at the ICR’s Centre for Protein Degradation combines TPD with personalised immunotherapy – another highly innovative drug approach that uses the body’s own immune system to fight cancer. This programme is expected to advance in 2026 into clinical trials for the treatment of paediatric brain tumours or paediatric solid body tumours. This is one of the first clinical examples of TPD application in childhood cancers – another major TPD milestone this year.”
Redefining radiation
Radiopharmaceuticals are an emerging class of targeted cancer treatments that combine a molecule capable of homing in on cancer cells with a radioactive agent, delivering lethal radiation precisely to tumours while sparing surrounding healthy tissue.
Recent advances have accelerated progress in this field. New radioisotopes are available, particularly highly potent alpha-emitters such as actinium-225 (Ac-225), which release large amounts of energy over very short distances. This makes them especially powerful at killing cancer cells while minimising collateral damage. At the same time, the targeting molecules used to guide these treatments to tumours have become increasingly sophisticated, improving accuracy and effectiveness.
At the ICR, researchers are exploring multiple radiopharmaceutical approaches across a range of cancers. One promising programme focuses on high-grade gliomas, including IDH-wildtype glioblastoma and paediatric-type diffuse high-grade gliomas, aggressive brain tumours with very limited treatment options. Preclinical studies of a novel targeted radiopharmaceutical, guided by immuno-PET imaging, have shown impressive results, raising hopes that this approach could soon progress into early-phase clinical trials.
Dr Gabriela Kramer-Marek, Leader of the Preclinical Molecular Imaging Group at the ICR, said:
“2026 is shaping up to be another big year for radiopharmaceuticals. There are several Ac-225-labelled molecules currently in development, with 13 already tested in humans, which gives a sense of how busy the pipeline has become. With several ICR-led programmes showing strong preclinical promise, we are hopeful that these approaches will move closer to the clinic and, ultimately, offer new options for patients with some of the hardest-to-treat cancers.”
An adaptive approach to accelerate brain cancer treatment
There have been over 1,000 brain cancer clinical trials over the past two decades, but there has been far less progress to treat the disease than in other cancers.
There are many hurdles to jump over when it comes to improving brain cancer treatments. The blood-brain barrier makes designing drugs that reach the brain difficult. Trialling drugs in these patients comes with many risks, as the brain is so fragile. And brain cancers are relatively rare, with small patient numbers meaning it takes many years to carry out clinical trials.
The 5G (next-Generation aGile Genomically Guided Glioma platform) study is a pioneering study aiming to drastically accelerate the process of finding new drugs for brain cancer. It is the world’s first adaptive clinical trial platform for patients with brain tumours. Patients will receive drugs based on the specific genetic makeup of their disease.
The first three arms of the trial are open, and it is in the process of being scaled up. Early results from the trial will be available at the end of the year.
“We were told the problem was too difficult. But we’ve done the pioneering work to build the 5G platform, we’ve started the trial, and I’m hopeful that we can soon make a change for patients with this devastating disease. This is just the beginning – I’m looking forward to the trial being scaled up, and I’m so excited to see the results from the three arms of the trial open currently.”
Boosting drug delivery
A major challenge for chemotherapy treatment is balancing the ability of the drug to kill cancer cells, with the damage it can cause to normal, healthy cells. Acoustic cluster therapy is an innovative approach designed to overcome this problem by enhancing the delivery of chemotherapy directly into the tumour.
The technology uses microscopic clusters of bubbles and liquid droplets that are injected alongside standard chemotherapy. A conventional ultrasound scan then converts the clusters into an activated form which, with further gentle ultrasound directed at the tumour, helps to pump the drug into the tumour, greatly increasing the amount of drug which reaches the cancer cells. Crucially, this could be used to increase the effectiveness of chemotherapy without increasing the dose given to patients.
A world-first clinical trial, led by researchers at the ICR and The Royal Marsden, tested this approach in patients with liver tumours that have spread from the bowel. This early-stage trial showed that Acoustic Cluster Therapy is safe, did not worsen the side effects of the chemotherapy, and helped improve the response of tumours to chemotherapy. A large multi-centre trial, including the ICR and The Royal Marsden, has now been opened to determine how Acoustic Cluster Therapy can boost treatment for locally advanced pancreatic cancer.
Professor Jeff Bamber, Professor in Physics Applied to Medicine, who led the work to develop and evaluate the technology at the ICR, said:
“Our innovative Acoustic Cluster Therapy is designed to overcome barriers to drug delivery that tumours develop. By doing so, it has the potential to both improve how well treatments work against tumours, while also lowering the frequency and severity of side effects. It could also enhance newer treatment approaches, including immunotherapy.
“The collaborative development and assessment of this technology highlights the ICR’s strong partnerships with industry in the field of medical imaging, and the unique environment we have for translating scientific advances into clinical trials. The Acoustic Cluster Therapy trials are examples of the ICR’s strength in working with The Royal Marsden, involving oncologists, radiologists, physicists and nurses working together to take research from ‘bench to bedside’ while supporting the patient through the treatment.”