Image: Staff nurse playing with a young boy in hospital. Source: Wellcome Images 2007. License: Creative Commons by-nc-nd 4.0.
Two single-letter changes to DNA are linked to an increased risk of B-cell precursor acute lymphoblastic leukaemia – one of the most common forms of childhood leukaemia – a new study has revealed.
The research, led by scientists at The Institute of Cancer Research, London, and published in the journal Nature Communications, also points to a possible biological mechanism behind the development of the disease.
The team analysed genetic data from almost 2,500 people with B-cell precursor acute lymphoblastic leukaemia, and more than 14,500 people without the disease.
By looking for consistent differences between the two groups, the researchers found two places where a switch of one letter of DNA was associated with a greater risk of the disease.
The two new single-letter changes bring the total known for B-cell precursor acute lymphoblastic leukaemia to 11. Together, these account for more than a third of the disease’s risk that is attributable to genetics.
The ICR's Division of Genetics and Epidemiology is internationally renowned for its pioneering work in understanding the underlying genetic causes of cancer risk.
Genetic links
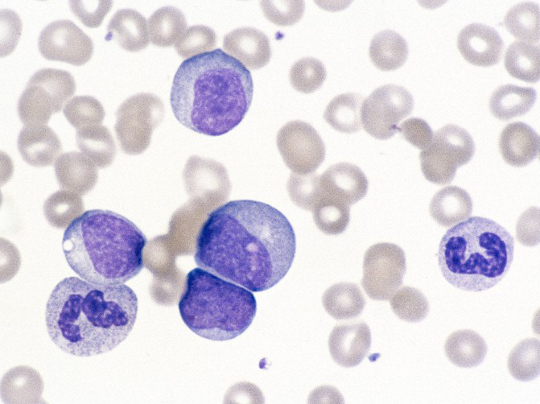
B-cell precursor acute lymphoblastic leukaemia is a cancer of the blood cells. People with the disease produce too many immature white blood cells, crowding out the production of other blood cells and leaving the person vulnerable to anaemia and infections.
By looking at all 11 single-letter changes found so far, the researchers tried to determine how these biological effects could arise from genetic factors.
They found that one variant is associated with an increased expression of a gene called PIP4K2A, thought to be involved in the regulation of cell production and maturation – both of which go wrong in B-cell precursor acute lymphoblastic leukaemia.
Another variant is associated with increased expression of the gene MYC, which helps regulate the expression of other genes. If these other genes are involved in cell growth and spread, this deregulation can lead to cancer.
Biological mechanism
Study leader Professor Richard Houlston, Professor of Molecular and Population Genetics at the ICR, said:
“This study expands our understanding of how genetic risk factors can influence the development of B-cell precursor acute lymphoblastic leukaemia, one of the most common forms of leukaemia in children.
“We identified two new genetic variants that increase a person’s risk of the disease, and provided evidence of a link between a number of these variants and expression of genes such as MYC and PIP4K2A – giving us a new insight into the biological mechanisms underlying the development of B-cell precursor acute lymphoblastic leukaemia.”