-by-yale-rosen-945x532.jpg)
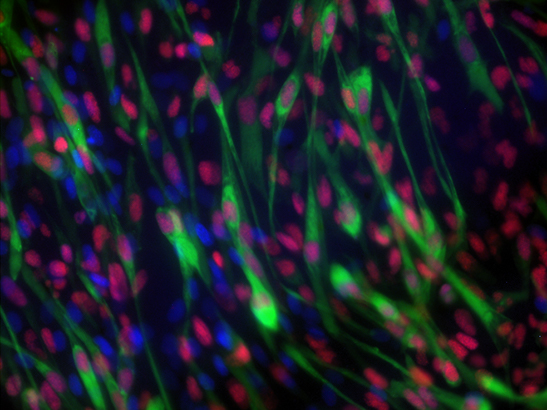
Image: Kaposi sarcoma (cropped image). Credit: Yale Rosen via flickr, CC BY-SA 2.0
One in two people in the UK develop cancer in their lifetime, so almost all of us are touched by the disease in some way. But still, many people who are diagnosed will be one of very few people with their cancer type. And some can be so rare, a person might never meet anyone else who has the same cancer.
Rare cancers are defined as affecting fewer than 6 in 100,000 people each year – yet together, they add up to 22 per cent of all cancer cases.
Bill Russell, aged 70 from Aylesbury in Buckinghamshire, is living with vascular sarcoma, a rare cancer of the cells that make up the walls of blood or lymph vessels.
Bill shared his experience: “There are not very many of us – people living with sarcoma. Healthcare professionals may only see one sarcoma in their working lives, and they occur in many different organs – which makes identifying them difficult.”
Aside from the importance of raising awareness of rare forms of cancer – even with doctors – the fact that not very many patients have these diseases comes with important challenges in finding new, better ways of treating them.
Practice changing clinical trials
This week, results from a clinical trial led by The Institute of Cancer Research showed that people with a rare cancer of the ureter and renal pelvis – starting in the tubes leading from the kidney to the bladder – could benefit from platinum-based chemotherapy after surgery.
The treatment halved patients’ risk of dying or the cancer coming back, giving them years more quality time with their families.
The results of the POUT trial are set to be practice-changing – but before embarking on the trial, the ICR scientists knew it would be challenging to gather enough data to draw meaningful conclusions.
Fewer than two in 100,000 people are diagnosed with cancer of the ureter and renal pelvis in the UK each year. So as not to miss out on any potential participants, the trial team put in a lot of hard work to identify and reach as many patients as possible who would be eligible, and invite them to join the trial.
Working closely with Dr Alison Birtle, the trial’s Chief Investigator at the Lancashire Teaching Hospitals NHS Foundation Trust, and the Trial Management Group made up of oncologists, urologists, clinical trials and qualitative researchers and patient representatives, the team managed to recruit 261 patients from more than 50 hospitals across the UK.
As it happened, the study didn’t end up recruiting the full number of patients they had originally aimed for – but they didn’t need to. Because the effect they were seeing was so strong, they could get statistically meaningful results from a smaller group of patients.
Professor Emma Hall, Professor of Oncology Clinical Trials and Deputy Director of the Clinical Trials and Statistics Unit at the ICR, was the Scientific Lead on the trial. She said:
“It’s fantastic to see such clear evidence of patient benefit from this study. It shows how important it is to run studies like this to improve treatment options for patients with rarer forms of cancer.”
Rethinking the clinical trial design
Compared with trials of more common cancers, clinical trials of rare cancers tend to involve a much larger number of hospitals – often internationally – and they usually need to be open for longer to ensure enough people can take part.
On top of this, trials may need to be designed differently to take into account the smaller numbers of patients.
In many clinical trials, patients are enrolled in one of two groups – with half the patients given the treatment under study, and the other half given the current standard of treatment.
But in the group of testicular cancer studied in another recent trial led by the ICR-CTSU, the results of which were published at the start of this year, this setup would have involved recruiting more than a thousand men – which would have taken much too long and would have made the trial far too costly.
As the study looked at halving the number of cycles of standard chemotherapy – for which the outcomes are well known – the trial team chose instead to recruit enough men to be able to rule out a relapse rate of 5 per cent or more.
They found that men could safely be treated with half the amount of chemotherapy to prevent their cancer from coming back – and the trial has already begun to change clinical practice.
Further barriers in children’s cancers
All childhood cancers are – thankfully – rare, making up less than 1 per cent of all new cancer cases in the UK. That means each year the lives of 1,900 children and their parents are upended by a cancer diagnosis.
The ICR carries out research into a range of children’s cancers and receives generous support from charities led by families affected by the disease.
Studying children’s cancers comes with similar challenges to those affecting other rare forms of the disease – but on top of these, children with cancer face further barriers in accessing clinical trials of new, targeted drugs.
Last year, scientists at the ICR found that half of children had genetic weaknesses in their tumours that could be targeted with existing adult cancer drugs – but only 7 per cent were able to access the treatment.
This touches on an important area of policy work for the ICR, which campaigns on issues ranging from age limits for clinical trials to regulatory barriers and incentives for pharmaceutical companies to test new cancer drugs in children.
We have a proven track-record of awe-inspiring research, which is transforming the lives of cancer patients around the world. This work is made possible by an extraordinary community of generous donors, which includes individuals, trusts and foundations and charity partners.
Pooling funding, resources and data
The small numbers of patients with each rare form of cancer are not just a challenge when recruiting for clinical trials – it’s also an important issue in fundamental discovery research.
As the ICR’s Dr Paul Huang told the BBC’s You, Me and the Big C podcast last summer, rare forms of cancer have historically received much less research investment than more common ones such as breast and prostate cancer. As a result, he explained, we are years behind in understanding the biology underlying rare cancers.
Dr Huang leads the Molecular and Systems Oncology Team at the ICR, which looks at different forms of sarcoma – rare cancers of connective tissue such as bone and muscle – characterising them on the basis of molecular and genetic features.
Now Dr Huang, together with Dr Robin Jones at The Royal Marsden and the ICR, will form part of a new international Sarcoma Accelerator Network announced last week.
Together with collaborators from across the UK and Europe, the network will build a digital hub of clinical and research data on sarcomas – using artificial intelligence to find new drug targets and ways to predict response to treatment.
Collaboration is key in rare cancers – to carry out the research itself as well as in how it’s funded. Collaborative models of funding involving government, academia, charities and industry are needed to take treatments for rare cancers forward into clinical trials.
And with funding for rare cancers often being more scarce than for more common cancer types, fundraising and philanthropy plays a particularly important role.
Dr Huang hopes to further expand the new sarcoma research project with philanthropic support, which would allow him to develop next-generation diagnostic tests to match sarcoma patients to the treatments most likely to work for them.
Big Data for a personalised approach
Pooling together research funds and efforts is one of the most important ways to tackle the unique research challenges posed by rare cancers – and in the age of personalised treatment, Big Data will start to make a big difference, too.
As we get better at identifying the genetics driving cancer types across the board, many new treatments are targeted at specific weaknesses in the tumour. Increasingly, people are starting to be offered drugs likely to work for them based on the genetic make-up of their tumour.
This is translating to a sense of momentum in studying rare cancers – with the new age of artificial intelligence and personalised treatment set to make a big difference.
With new approaches like AI to crunch data, we’re gaining an ever-growing understanding of the biology underlying the more than 200 different kinds of rare cancers.
As Dr Huang said,
“We’re working towards a future where rare cancers are no longer complex diseases, but ones where we really understand the biology – and where we can design smarter clinical trials to deliver drugs to our patients.”