Two studies have uncovered how combining a cancer-killing reovirus with targeted cancer drugs can dramatically boost immune responses and tumour destruction – offering a promising route to more effective, personalised cancer therapies.
Researchers at The Institute of Cancer Research, London, have shown that this combination involving virotherapy – where viruses are converted into a cancer treatment – can trigger powerful immune activation and cancer cell death, both in lab-grown cells and in mice.
The findings, separately published in Nature Communications in May 2025 and July 2025, highlight how reprogramming how the tumour responds to stress and signals from the body’s immune system can unlock new therapeutic potential from existing drugs.
These research studies were led by Professor Kevin Harrington, Professor in Biological Cancer Therapies at The Institute of Cancer Research (ICR) and a consultant oncologist at The Royal Marsden, and funded by a Cancer Research UK programme grant.
Rewiring cancer’s stress response
Oncolytic viruses are types of viruses that can infect and destroy cancer cells, while leaving healthy cells unharmed. The oncolytic virus in question for these two studies, called a reovirus, which was provided by Oncolytics Biotech for both studies, is a naturally occurring double-stranded RNA virus. It selectively infects and kills cancer cells, which have weakened antiviral defences – making them more vulnerable to infection.
In both studies, researchers utilised high-throughput drug screening to identify compounds that could enhance the effects of the reovirus. Two drugs – talazoparib and palbociclib – stood out as especially powerful partners for the virus, each working in a different way to boost its cancer-killing effects
In the talazoparib study, the research team discovered that the reovirus activates a protein called PARP-1, which normally helps cells survive stress. Stopping the function of PARP-1 with talazoparib, a PARP-1 inhibitor, disrupted the cancer cells’ defences, triggering stronger cell death and immune activation. The combination was also seen to amplify the production of key immune-stimulating molecules – important messengers that help rally the immune system to attack cancer cells. In mouse models, this dual therapy not only shrank tumours but also prevented their return, suggesting the immune system had developed a memory of the cancer.
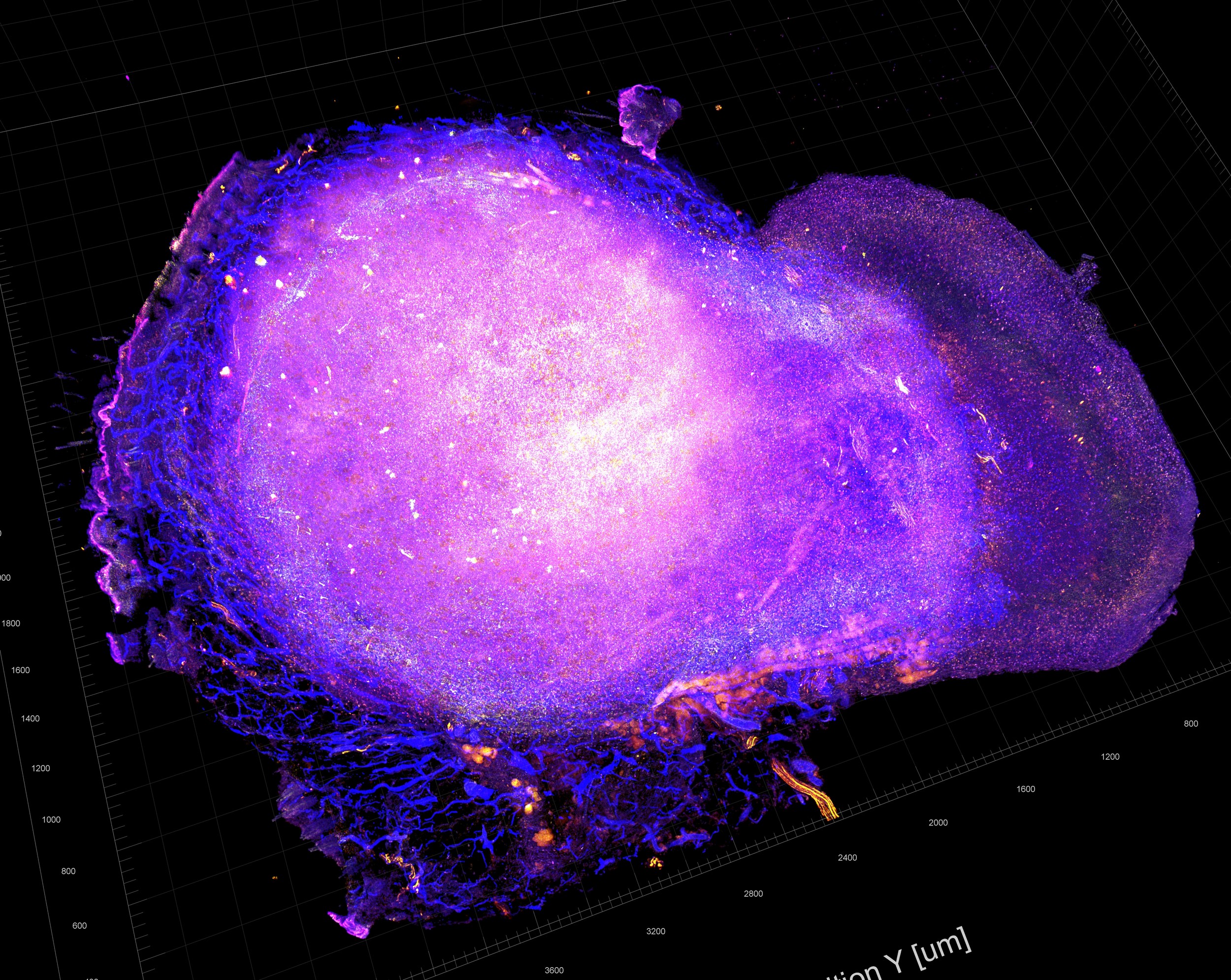
Meanwhile, the palbociclib study revealed that the drug enhances reovirus-induced endoplasmic reticulum stress – a form of cellular stress that can trigger immune activation. The combination boosts production of immune-stimulating molecules, increasing the expression level of antigen-presenting molecules and altering the peptides associated with them.
These changes made cancer cells more visible to the immune system and led to a stronger infiltration of immune cells. In mouse models, the combination also led to reduced tumour growth and increased immune cell activity, suggesting the treatment could help train the immune system to fight cancer more effectively.
Unlocking immune visibility
Both studies highlight the importance of pattern recognition receptors – which detect viral RNA and initiate immune responses to help the body recognise and attack cancer cells – such as RIG-I. Reovirus activates RIG-I, and both talazoparib and palbociclib appear to enhance the immune response – either by blocking a protective molecule that helps cancer cells survive (in the case of talazoparib) or by amplifying stress signals (palbociclib). This triggers a wave of immune activation, helping the body recognise and respond to the cancer more effectively.
Importantly, the research team showed that similar effects could be achieved using non-viral RNA therapies and molecules that activate RIG-I, suggesting that the therapeutic benefits of these combinations could extend beyond reovirus itself.
Towards smarter, personalised therapies
Image: The Tareted Therapy Group, including Victoria Roulstone (second from the right) and Kevin Harrington (centre).
Both talazoparib and palbociclib are already approved for use in certain cancers, such as breast cancer, and the Type 3 (Dearing) strain of reovirus is currently under clinical investigation. The research team are now exploring how these combinations of reoviruses and targeted therapies could be tested in early-phase clinical trials, potentially alongside immune checkpoint inhibitors.
Co-first author of both studies Dr Joan Kyula-Currie, Senior Scientific Officer in the Targeted Therapy Group at The Institute of Cancer Research, said:
“These findings show how we can harness the body’s own immune defences by combining oncolytic viruses with targeted drugs. By understanding the molecular interaction between stress pathways and immune sensors, we can design smarter, more effective cancer treatments.”
Co-first author of both studies Dr Victoria Roulstone, Senior Scientific Officer in the Targeted Therapy Group at the ICR, said:
“This work highlights the power of combining virotherapy with targeted drugs that modulate the tumour environment – unlocking entirely new ways to kill cancer. It’s an exciting step towards more personalised and immune-driven cancer treatments and I hope we’re able to see these discoveries turned into early-stage clinical trials to test whether these combinations work just as effectively in patients.