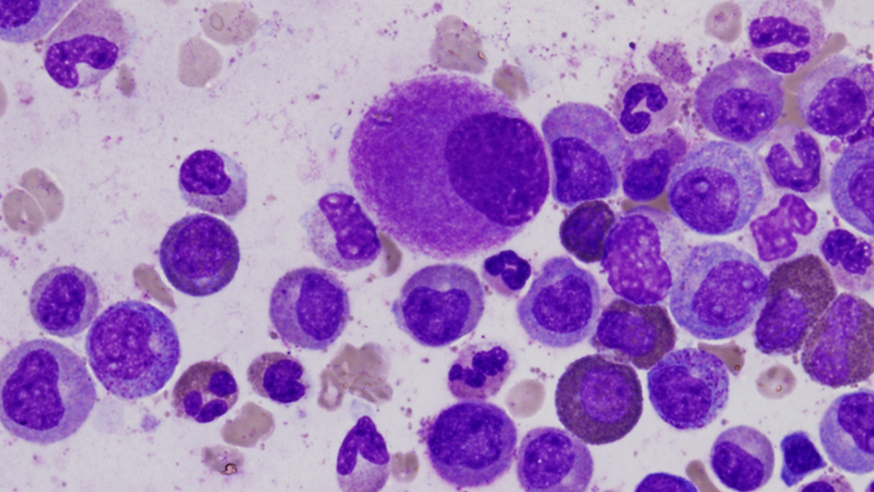
Deformed cells in the bone marrow, typical of chronic leukaemia (photo: Difu Wu)
Researchers have found a way to estimate the number of cells responsible for driving and maintaining a cancer’s growth. The results could help to tailor treatments to each patient’s cancer.
The study used mathematical models to predict the amount of cancer stem cells – cells that can renew themselves and drive tumour growth – that exist in different cancers.
Understanding how cancer stem cells are driving a patient’s cancer could help doctors choose the most appropriate treatments.
The findings were published in Cancer Research. The study received funding from the Wellcome Trust, the Geoffrey W. Lewis Post-Doctoral training fellowship, the Chris Rokos Fellowship and the Deutsche Akademie der Naturforscher Leopoldina.
Researchers combined mathematical modelling and measurements taken in the clinic to predict the numbers of cancer-driving stem cells in tumours from patients with chronic myeloid leukaemia – a type of blood cancer.
Estimates of cancer stem cells were calculated from the growth and reduction of tumour size before and after treatment with the targeted drug imatinib.
Based on patient responses, researchers predicted that after one year of targeted treatment the number of cancer stem cells remains approximately constant, although the tumour reduces by about 100-fold.
Modelling 'could guide treatment'
Even five years after continued treatment, and an approximate 1000-fold reduction of the total tumour, the number of cancer stem cells decreases only very slowly.
Study leader Dr Benjamin Werner, a postdoctoral training fellow in the Evolutionary Genomics and Modelling team at the ICR’s Centre for Evolution and Cancer, said: “We believe that cancer stem cells make up only a very small fraction of the tumour, but we do not know how many are present in each cancer type, or how many of these cells are needed to drive a tumour in a specific patient.
"Our study shows that it could be possible to estimate these numbers from measurements that are routinely taken from medical imaging or liquid biopsies. In future, we hope to apply the same method to solid tumours to see if the behaviour is similar.”
This type of modelling could potentially be used to guide treatment that is tailored to each patient.
Dr Werner explains: “Cancer stem cells not only drive cancer growth, but they can be highly resistant to radio- and chemotherapy. Estimating the number of cancer stem cells at diagnosis and during treatment could influence how aggressively we need to treat the cancer, for how long, and what types of drug combinations will be the most effective.
"For instance, patients with only few remaining cancer stem cells might benefit from treatment discontinuation, while patients with a high number of cancer stem cells would benefit from changing the treatment strategy.”