_kevin-harrington-embed.jpg)
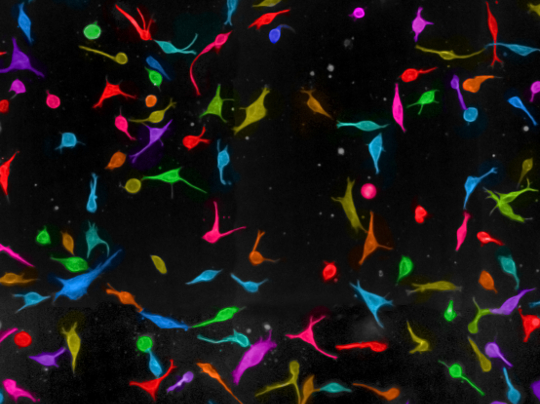
T-vec infected melanoma cells. Credit: Professor Kevin Harrington
A cutting-edge form of non-invasive imaging technology can track the response of malignant melanoma cells to treatment, researchers have found.
The results suggest that both photoacoustic imaging and magnetic resonance imaging could be used to measure the effectiveness of targeted cancer drugs.
Photoacoustic imaging (PAI) technology shines laser pulses on to objects, and produces images by analysing the ultrasonic sound waves they emit in response.
Magnetic resonance imaging (MRI) is an existing technology which scientists are developing in new ways to see inside tumours, and monitor the effect of drugs.
Using PAI and MRI, a research team at The Institute of Cancer Research, London, was able to detect changes in melanoma cells as a result of treatment with two targeted drugs.
The scientists reasoned that both technologies might be able to tell whether melanoma cells were responding to drugs because effective treatment increases the levels of dark pigment melanin, which absorbs light.
They sought to measure melanin increase in cells using either imaging modality: by increased laser beam absorption in PAI, or by changes in the magnetic environment via MRI, caused by the effect of melanin on magnetic iron.
Imaging differences between cells
Writing in the journal Scientific Reports, the researchers explained how they measured the changes in melanin levels prompted by two drugs: vemurafenib, which targets a protein called BRAF, and Hsp90 inhibitor 17-AAG.
They treated melanoma cells with each drug, producing images after each treatment and comparing them with images produced using untreated cells. They confirmed that measurements showing melanin increases were correct using standard laboratory tests.
The research, which was funded by a range of organisations including Cancer Research UK, the Medical Research Council and the Engineering and Physical Sciences Research Council, showed that both PAI and MRI could be used to monitor treatment effectiveness.
The researchers also discussed the relative advantages and disadvantages of each type of technology for future use in patient care.
MRI is a well-established technology offering detailed imagery, but is relatively expensive to carry out. PAI could be more cost-effective as an extension of ultrasound scanning, and integrate with other forms of imaging in multi-imaging tests – but is still an emerging technology which can only currently produce images from a limited depth.
Research at the ICR is underpinned by generous contributions from our supporters. Find out more about how you can contribute to our mission to make the discoveries to defeat cancer.
Potential for patient follow-up
Study leader Dr Mounia Beloueche-Babari, Staff Scientist working in the Cancer Research UK Imaging Centre at the ICR and The Royal Marsden NHS Foundation Trust, said:
“It’s important to find improved ways of monitoring the effectiveness of targeted cancer drugs. Some drugs – like BRAF inhibitors – play an important part in current treatment but often stop working after a few weeks or months, and in the future we want patients to be able to move between treatments as effectively as possible.
“With more research, we hope that this use of photoacoustic and magnetic resonance imaging could be adapted for use in patients, making it easier to identify who is responding to drugs, and who might be better off moving to another treatment.”
Study co-author Professor Jeffrey Bamber, Professor in Physics Applied to Medicine, and Team Leader in Ultrasound and Optic Imaging at the ICR, said:
“The PAI scans, conducted by Dr Anant Shah in my team, have shown that photoacoustic imaging – an emerging technology that uses an ultrasound scanner to measure the sound waves emitted by tissues illuminated by short and safe pulses of light – can detect drug-induced changes in melanoma cells.
“Magnetic resonance imaging technology can also detect these changes, which are caused by increased levels of the pigment molecule melanin.”