Video: Dr Ben O’Leary discusses a new blood test for women with advanced breast cancer which can predict how well patients will respond to a new drug right at the start of treatment.
A new blood test for women with breast cancer can predict how well patients will respond to a new drug right at the start of treatment.
The new blood test detected genetic changes within women’s breast cancers which indicated that these patients were less likely to respond to treatment – and that their disease could be expected to come back quickly.
Targeted drugs have shown benefit for many women with advanced breast cancer, but some patients stop responding soon after starting treatment as their cancer evolves to become drug resistant.
In future, the new test could help identify nearly half of women with the most common form of breast cancer who are at the highest risk of early relapse – who will need further trials of new treatments to stop their cancer becoming resistant – as well as identifying those who will do very well on treatment.
Many scientists from The Institute of Cancer Research, London are attending the 2019 ASCO conference in Chicago. See all of our news, blog and video content from the event.
Early relapse
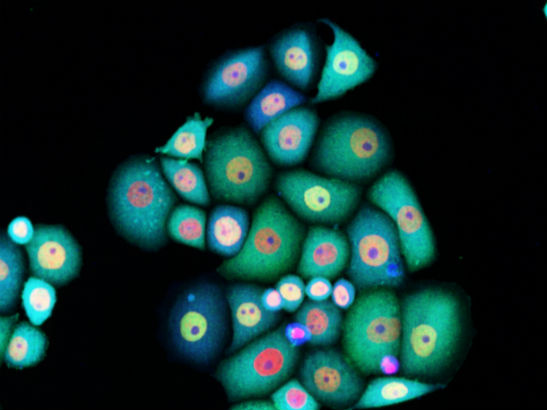
Scientists at The Institute of Cancer Research, London, analysed fragments of cancer DNA that have entered the bloodstream to study the effect of genetic changes in a woman’s tumour – often called liquid biopsies.
They took blood samples from 310 women with oestrogen receptor positive breast cancer – the most common form of the disease – who were taking part in a clinical trial of palbociclib and fulvestrant for advanced breast cancer.
The team found that 131 women – 42 per cent – had one or more of three changes in the tumour DNA circulating in the bloodstream that put them at risk of early relapse.
The research, presented today (Saturday) at the 2019 ASCO Annual Meeting in Chicago, was funded by the Medical Research Council, Breast Cancer Now, and the manufacturer of palbociclib, Pfizer.
The p53 gene
Researchers at The Institute of Cancer Research (ICR) – a charity and research institute – and The Royal Marsden NHS Foundation Trust examined the impact of specific genetic changes within patients’ cancers at the start of treatment.
Women whose circulating tumour DNA contained changes in the well-known cancer gene, p53, saw their cancer come back after an average of 3.7 months, compared with 12.7 months in women without p53 gene changes.
An increase in the number of FGFR1 gene copies and a high level of tumour DNA in the bloodstream also shortened the average time before a woman’s cancer came back.
Women with these changes in circulating tumour DNA saw their cancer return after an average of 3.9 months compared with 12 months in women without these changes.
The study also found a link between faults in the p53 gene and the number and location of sites in the body to which cancer had spread.
Next, the blood test needs to be evaluated as part of different clinical trials to assess its value in other groups of patients, before it can start benefiting women with advanced breast cancer in the clinic.
The research follows a recent announcement by the ICR of a £15 million fundraising drive to complete a new £75 million Centre for Cancer Drug Discovery focusing on overcoming cancer evolution and drug resistance.
Predicting cancer's next move
Professor Nicholas Turner, Professor of Molecular Oncology at The Institute of Cancer Research (ICR) and Consultant Medical Oncologist at The Royal Marsden, said:
“Exciting new targeted treatments like palbociclib are beginning to have a real impact on survival for women with breast cancer, but unfortunately many tumours which initially respond will later develop resistance and come back.
“Our study found that a new genetic test could detect right at the start of treatment those women whose cancers were most likely to develop resistance quickly to palbociclib. We could then adjust their treatment plan accordingly – trialling additional treatments from the outset to try and prevent resistance, or planning for a switch to another treatment as soon as resistance develops. We now need to assess in a clinical trial whether helping direct women’s care with this new test can offer improved survival and quality of life.”
We are building a new state-of-the-art drug discovery centre to create more and better drugs for cancer patients.
Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said:
“Cancer’s ability to evolve to become resistant to treatment is the greatest challenge we face in improving patients’ survival and quality of life.
“So-called liquid biopsy tests like this one are a key part of our toolkit in staying on top of cancers’ adaptability and evolution, and picking up the earliest signs of drug resistance. Detecting the potential of cancers to evolve resistance could allow us to predict cancer’s next move and to respond with adaptable new treatment plans.
“This study is a demonstration of the exciting new ‘Darwinian’ approach to treatment we will be taking once we have raised the money to complete our new £75 million Centre for Cancer Drug Discovery.”
More ASCO coverage
- Patients put at the forefront for world’s largest cancer conference
- Drug targeting DNA damage response shows promise against cancers of anus and genitals
- Immunotherapy better than aggressive chemotherapy as first treatment option for recurrent head and neck cancer
- Breast cancer drug effective in 80 per cent of men with BRCA-mutant prostate cancer
- ICR research makes waves at world’s largest cancer conference