Infectious diseases like smallpox, polio and tuberculosis used to cause huge amounts of death and disability across the world, but the advent of vaccination has all but wiped out them out.
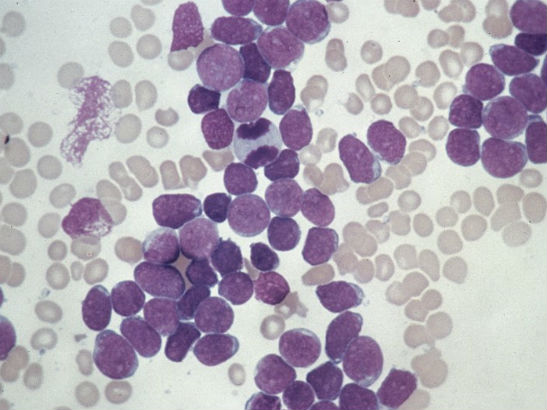
Immunisation is one of the great successes of modern medicine and has helped to protect millions of lives. But there is also an interesting, unusual and perhaps paradoxical link between infections and the most common form of cancer in children, called acute lymphoblastic leukaemia (ALL).
It has long been suspected that infections are the most likely cause of leukaemia, and various epidemiological studies have shown that recurring infections during childhood are linked in some way to the development of ALL – but it’s complex.
Research by scientists here at The Institute of Cancer Research in London, backed up by studies carried out worldwide, has shown that mixing with children in the first years of life in crèche or day-care, and experiencing the normal coughs and sneezes of the group, can greatly reduce the chances of a child developing ALL.
So it seems likely that something about the building up of the immune system – either through vaccination or through exposure to common infection – is likely to prevent ALL. Quite how this happens has been unclear, however.
'Infections could be a trigger'
Now Professor Mel Greaves here at the ICR, a world-leading expert in childhood leukaemia and Director of our Centre for Evolution and Cancer, has worked with an international team of scientists on a study that provides some important clues. It shows how some infections could cause ALL in children.
The new research, published in Nature Immunology, describes how infection might instigate harmful mutations to mouse DNA through two enzymes called AID and RAG. It is this collateral damage that may in turn trigger ALL.
Professor Greaves has studied ALL extensively, and proposed the hypothesis more than 25 years ago that ‘delayed infection’ could be a major cause of leukaemia.
The idea suggests that exposure to infection in the first years of life helps to protect against leukaemia, and tallies with higher incident rates for the disease in more affluent societies – where hygiene is easier to maintain.
The absence of these early infections means that our immune systems are not primed for more serious infections later on, and it is this that ultimately leads to the mutations that cause ALL.
This idea assumed that there is some ‘pre-leukaemic’ cell, from which ALL originates, and Professor Greaves helped to identify the founding mutation in ALL, which occurs in children before they are born.
The mutation, a fusion of two genes called ETV6 and RUNX1, develops in white blood cells called B-cells, which form part of our immune system and make antibodies to fight infections.
But even with this mutation, less than 1% of children go on to develop ALL, so other mutations are also needed for the disease to develop.
Finding the mutation's missing link
Now, Professor Greaves and colleagues have found the missing link in how this mutation in the womb leads to ALL.
Previous research by Professor Greaves connected a key mechanism in the immune system to ALL. The study, published last year in Nature Genetics, identified the enzyme RAG – which is normally involved in creating genetic diversity in the production of antibodies – as being the main driver of the disease in 57 patients with ALL.
It found that genomic rearrangements and deletions of DNA segments were important steps in the development of cancer, and that each patient studied showed evidence of events involving RAG.
But for ALL to develop, another enzyme that is only very transiently made in cells, called AID, also has to play a role.
The new study showed that infection can activate the enzyme AID and, in combination with RAG, promote the evolution of the disease by triggering mutations in pre-leukaemic B-cells.
In cells treated to promote AID activity, they found that inflammatory signals, which are often triggered by infection, significantly boosted the number of cells producing both AID and RAG.
In mice, switching off either AID or RAG prevented inflamed cells from developing into ALL, whereas in mice with normal AID and RAG activity, inflammation caused terminal ALL to develop within three weeks.
The study reveals the mechanism by which common infections can trigger childhood ALL in susceptible individuals and how paradoxically, natural infections acquired in infancy through exposure to other children may serve to prevent the disease. This mechanism could also be triggered by a small number of vaccinations.
By understanding how infections contribute to ALL, we could also work out which infections are the most harmful, and hopefully stop more children from developing this harrowing disease.