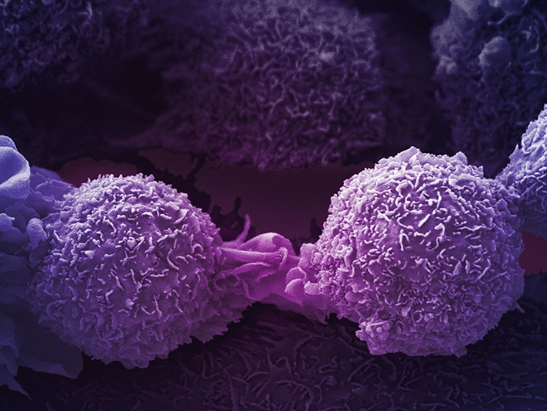
Image: Lung cancer cells. Credit: Anne Weston, Francis Crick Institute. CC BY-NC 4.0
Cancer cells are able to grow, spread and resist treatment by the process of ‘evolution’. Evolution is often seen as an invisible process involving gradual change over time and resulting in some sort of advantage.
Think of humans evolving from primates, a process that took millions of years – but with cells and over a much shorter timescale.
As a tumour cell divides, it can undergo genetic changes that affect what it is capable of doing. These genetic changes can make cells divide out of control or ignore standard signals from the body instructing them to die. And some genetic changes can even help tumour cells avoid the immune system, our body’s main line of defence.
At the ICR, Dr Yinyin Yuan and her team are working on the TRACERx project, a multi-million pound initiative funded by Cancer Research UK, led by colleagues at UCL and The Francis Crick Institute, and involving collaborators at many other centres.
Their research, which aims to harness the principles of evolution to stop cancer in its tracks, has transformed our understanding of how lung cancer evolves over time – and has highlighted how big a role the immune system plays in cancer evolution.
“Our TRACERx research has helped us gain insight into how lung cancers can cloak themselves to escape the attention of the immune system – and in doing so can continue to evolve and develop,” says Dr Yuan.
How cancer evolves and relapses
At the start of treatment, it is possible that all cancer cells in a tumour are the same and responsive to a drug. But in some cases, one of those cells may undergo a genetic change – a mutation – that makes it resistant to treatment.
Even if the drug kills most of the cancer cells, a small group of newly mutated cancer cells can evade treatment and survive, thanks to the genetic changes that make them resistant. In advanced cancers, the resistant cells can take advantage of nutrients and space left behind by the other cancer cells killed by the drug – spreading, invading new organs and becoming unstoppable.
When the majority of cancer cells become resistant and fail to respond to treatment, the patient relapses.
Cancer evolution relies on the build-up of these genetic changes and it is the greatest challenge faced by cancer scientists – but evolutionary thinking also holds the key to solving the problem.
Understanding the immune landscape
Evolution responds to shifting surroundings. For instance, it would be hard to figure out how and why primates gradually evolved into humans if we didn’t know much about the environment that triggered the shift from knuckle-walkers to bipedal animals that can walk and run upright and on two feet.
Bearing in mind the huge role the environment can play in evolution, our scientists are studying the types of immune landscapes that enable tumours to grow.
Tumours’ immune environments can differ. They can be filled with immune cells, or have almost none. Sometimes you can have a mixture, with ‘hot’ regions full of immune cells and ‘cold’ regions with sparse immune cells.
As part of the TRACERx initiative, Dr Yinyin Yuan and her team have applied machine learning to genetic data and pathology images to create an AI tool capable of distinguishing immune cells from cancer cells. This creates a detailed picture of how lung cancers evolve in response to the immune system in different patients.
They believe that cancer cells in immune ‘cold’ regions may have evolved more recently than cancer cells found in immune ‘hot’ regions. These immune cold regions are therefore associated with cancer relapses – meaning that areas of the tumour with fewer immune cells may have developed a ‘cloaking’ mechanism under evolutionary pressure from the immune system, allowing them to hide from the body’s natural defences.
The hope is that this AI tool could be used in the future to pick out lung cancer patients at highest risk of relapse, helping inform a more tailored treatment strategy.
Mapping the evolution of lung cancer
“Our research is helping us understand why some lung cancers are so difficult to treat,” says Dr Yuan.
“We’re trying to figure out what impact the immune system is having on cancer evolution and aiming to get a clear picture of the complex relationship between lung cancer and the immune system.
“By improving our understanding, we might be able to target cancer’s ability to evade the immune system – potentially coming up with ways to reactivate immune cells and encourage them to go after sly cancer cells, for example.”
While TRACERx research focuses on four cancer types – lung, melanoma, prostate and renal cancer – Dr Yuan’s team specifically studies lung cancer. Her team’s research is bringing us closer to an era of precision medicine for this cancer type, which remains, by far, the biggest cancer killer in the UK.
Lung cancer’s high mortality rate is partly due to its ability to evolve, become resistant to treatment and relapse, so it’s very encouraging to see our scientists making strides in this field by attempting to understand lung tumours as evolving ecosystems.
The ICR’s new Centre for Cancer Drug Discovery has now been completed and our researchers have now moved into the new building to carry out all kinds of research aiming to tackle cancer’s lethal ability to evolve resistance to treatment – so watch this space!