Search Issue 51 | Spring 2025
Editorial
Our mission to defeat cancer would not be possible without the continuous commitment of both our staff and our supporters, whose inspiring efforts lead to inspiring science.
In recent months, staff members have climbed mountains not only figuratively for the ICR – through their dogged pursuit of scientific answers – but also literally. Dr Rachael Natrajan cycled the Italian hills between Venice and Rome, while Professor Helen McNair trekked to the K2 Himalayan basecamp. Several employees also joined more than 100 walkers in the hilly Lake District for Climb of Life – now in its 18th year supporting us.
We also continue to be in awe of the generosity of our supporters. The Doing it for Daniel Foundation donated £21,000 to fund vital research by Professor Chris Jones in paediatric brain tumours –particularly diffuse midline glioma, the terminal brain stem cancer that affected Daniel. We are eternally grateful for their support.
In the labs, our scientists are making progress against many different cancer types. Head and neck cancer, which has seen few curative advances, is the focus for Dr Ben O’Leary, who was recently appointed to lead the Evolution and Translational Genomics Group. We are also seeing encouraging developments in blood cancer due to the ground breaking research advances made by our scientists.
As ever, we remain at the forefront of cancer research –thanks to our staff, students, supporters and partners. Together, through passionate fundraising efforts and the unwavering determination of our scientists, who challenge conventions to drive breakthroughs in drug discovery and development, I believe we can defeat cancer.
Professor Kristian Helin
Chief Executive, The Institute of Cancer Research
Research news
Improved breast cancer diagnostic tools on the horizon
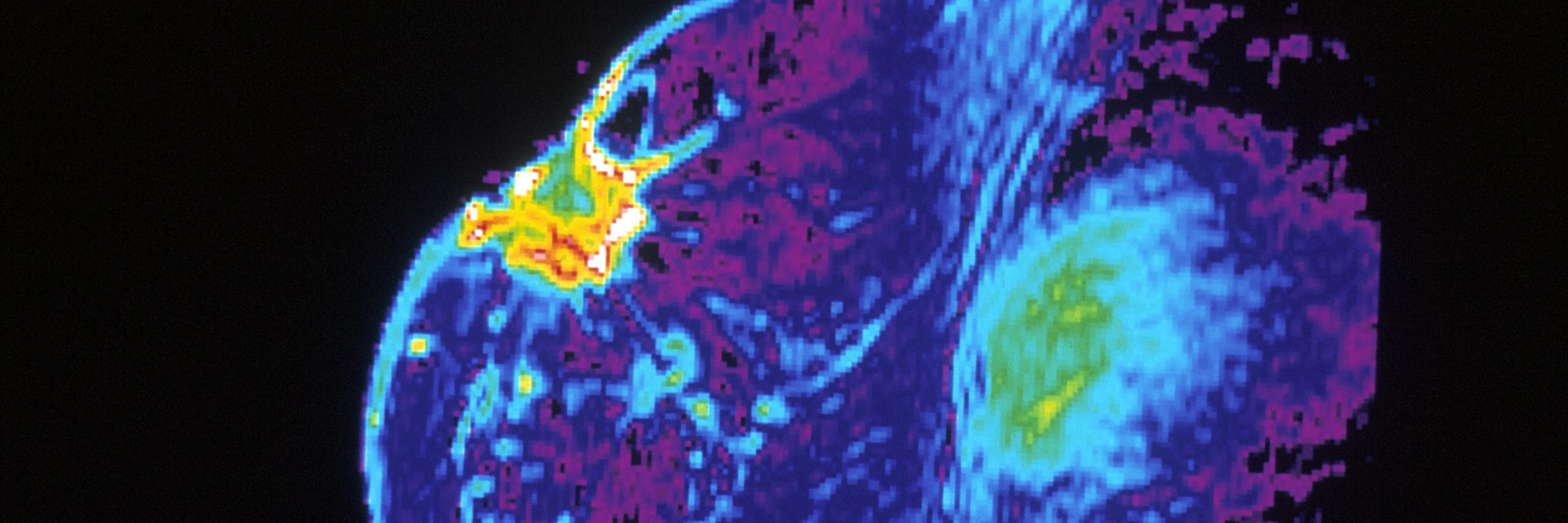
Our scientists, having led one of the world’s largest and longest-running studies into the causes of breast cancer, have developed tools to identify women at high risk of the disease, even if they don’t have a family history.
Our scientists are developing tools that will help to identify women at high risk of breast cancer, even if they do not have a family history of the disease.
The Breast Cancer Now Generations Study is one of the world’s largest and longest-running studies into the causes of breast cancer. Over the past 20 years, it has contributed to the discovery of hundreds of genetic changes linked to breast cancer and shed light on the major associated lifestyle and hormonal factors.
Study co-leader Professor Montserrat Garcia-Closas said: “We're going to develop better breast cancer risk assessments by building on the discoveries made over the last two decades into the genetic, social and environmental factors that cause breast cancer. This will help women receive more personalised and effective care.”
“We're going to develop better breast cancer risk assessments by building on the discoveries made over the last two decades.”
New drug target discovered for aggressive form of prostate cancer
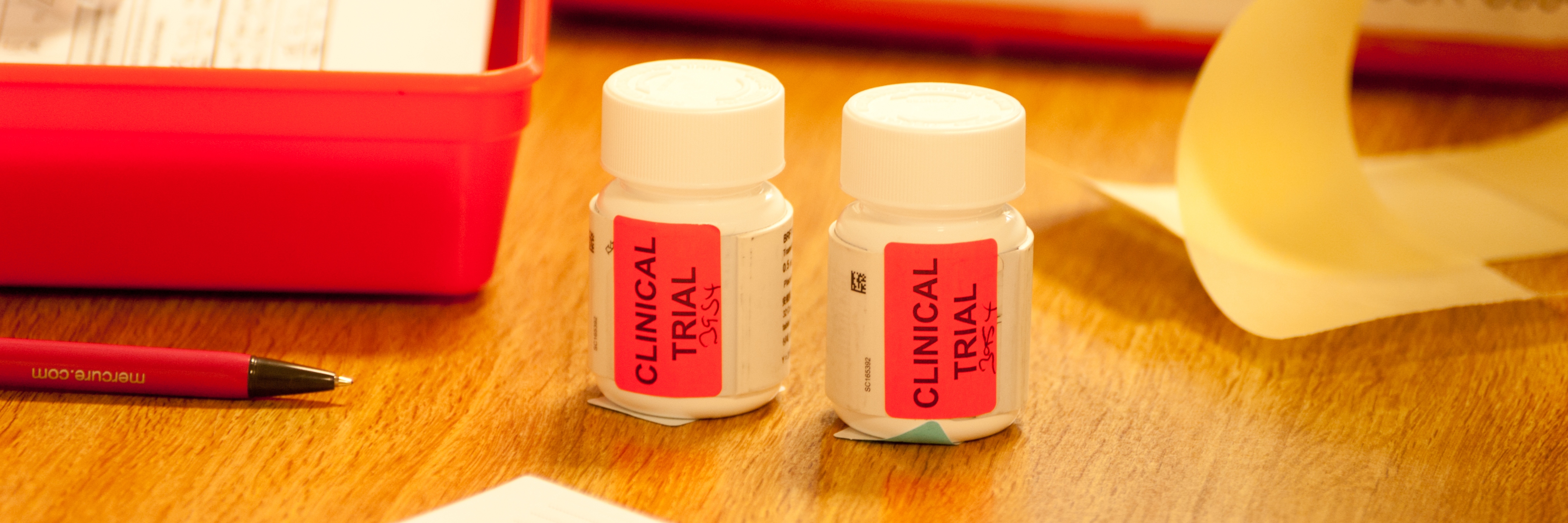
Our scientists have discovered that a protein linked to prostate cancer is associated with more aggressive forms of the disease. In new research led by Professor Johann de Bono and Dr Adam Sharp, the team has shown that the BCL2 protein is present in high levels in a type of advanced prostate cancer that has stopped responding to hormone therapy.
It is now hoped that BCL2 could be a new target for treatment and be used to help predict who will become resistant to hormone therapy. A prostate cancer clinical trial testing the BCL2 inhibitor venetoclax – a drug approved for some types of leukaemia – along with the hormone therapy enzalutamide has already begun.
Advance
Tackling all types of blood cancer is key to improving outcomes for patients
Blood cancer is an umbrella term for cancers of the blood, bone marrow and lymphatic system. A new diagnosis occurs every 14 minutes, making it the fifth most common cancer in the UK. It also has the third highest mortality rate.
Despite these statistics, blood cancer receives less attention at a national level than common solid tumour cancers, such as breast, prostate and colorectal.
This is largely because different types of blood cancer are reported on separately. Individually, each causes fewer cases and deaths than blood cancer would overall, masking the disease’s real impact.
Blood cancer poses some unique challenges
Nonspecific symptoms, including unexplained weight loss, bruising and fever, mean blood cancer often goes undiagnosed until it has progressed. Also, while solid tumours have fixed positions initially, blood cancer circulates the body. Some standard cancer treatments – including surgery and radiotherapy – are therefore not suitable.
Undaunted by these hurdles, our scientists are working hard to find better ways to diagnose and treat blood cancer. Their projects span multiple blood cancers, including the three main types: leukaemia, lymphoma and myeloma.
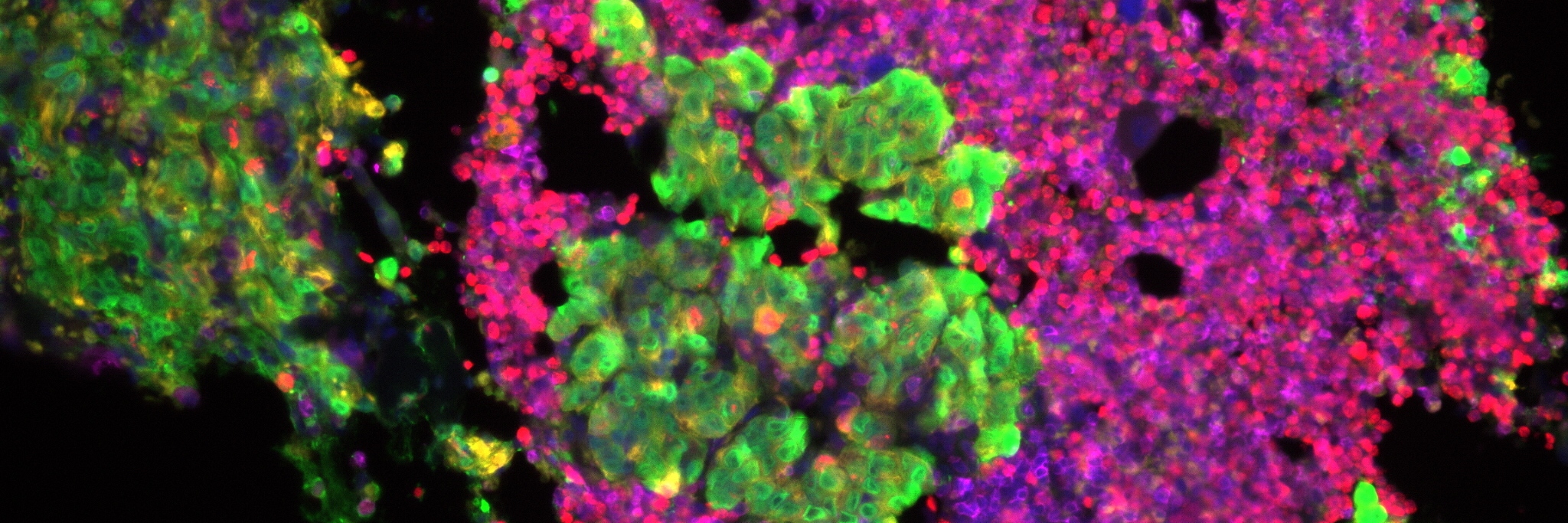
Identifying an untapped vulnerability in leukaemia
A team led by Professor Kamil Kranc, Professor of Haemato-Oncology, has developed a new treatment approach for acute myeloid leukaemia (AML), an aggressive blood cancer lacking treatment options.
In a recent preclinical study, scientists showed that blocking enzymes called PHDs causes protein level changes that stop AML from starting or progressing. They then generated a PHD inhibitor called IOX5, which uses a unique mechanism to selectively block PHDs. The next step is to progress this compound to clinical trials. Encouragingly, existing anaemia drugs that block PHDs have also been shown to be effective, so multiple new leukaemia treatments could be on the horizon.
“A new diagnosis occurs every 14 minutes.”
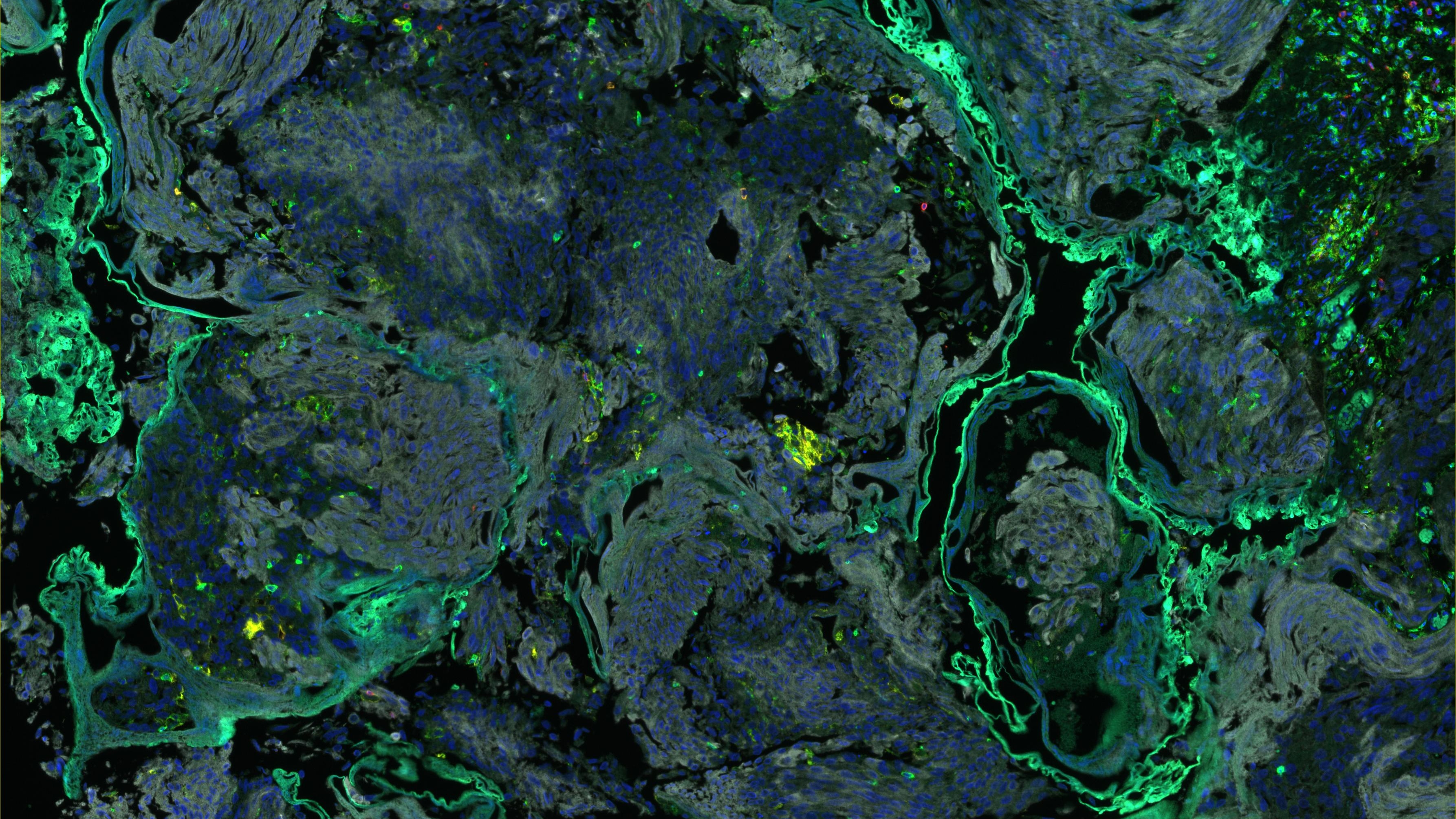
Focusing on lymphoma at the drug discovery stage
Several of our teams have helped develop a compound with the potential to treat B-cell lymphoma and other cancers. Dr Rob van Montfort’s Hit Discovery and Structural Design Group first discovered new small molecules able to block a protein called BCL6. BCL6 binds to and helps switch off target genes involved in cell division and cell death, promoting cancer growth.
Professor Swen Hoelder, Head of Chemistry, and his colleagues in our Centre for Cancer Drug Discovery then created a potent compound that binds to BCL6 and tags it for destruction – a process called protein degradation. This compound successfully inhibited lymphoma cell growth. The team now plans to test it in further preclinical studies.
A potentially practice-changing trial in myeloma
Our researchers co-led MUK Nine OPTIMUM, a first-of-its-kind myeloma trial that compared patient outcomes across two clinical trials rather than using a control group. All the patients had ultra-high-risk myelomas, which have certain genetic changes that make them more aggressive.
The first trial, Myeloma XI (MyXI), used the standard of care – a quadruple therapy – while the second, OPTIMUM, tested a combination of five drugs, three of which were not part of the standard treatment.
The study showed that the OPTIMUM participants were, on average, more likely to have a good outcome. At a 30-month follow-up, 77 per cent had stable disease that was unlikely to progress soon, compared with 39.8 per cent of the MyXI participants.
The scientists, led by Dr Martin Kaiser, Group Leader in Myeloma Molecular Therapy, hope the new drug combination can be made available to high-risk patients with myeloma.
A promising future
Although overall blood cancer survival rates increased by 14 per cent between the 1994–2007 and 2008–2021 periods, some types – such as AML – are still very deadly, meaning much work remains to be done.
Fortunately, cancer research is arguably more dynamic than ever before, with discoveries being made at an unprecedented rate and the understanding of cancer increasing daily.
We remain at the forefront of this research, with our scientific breakthroughs helping develop new diagnostic tests and treatments. We are determined to give blood cancer the attention it needs so that we can improve patient outcomes and save thousands more lives.
Fundraising focus
“Every child with brain cancer should have a chance at life”

Daniel Caplan was 16 when he was diagnosed with an aggressive brain tumour. He passed away seven months later. Last May, to mark what would have been his 21st birthday, his parents Alison and Brian generously donated £21,000 to fund our research. Here, Alison explains why she hopes her son’s legacy will improve treatments for young people with cancer.
“Daniel was vibrant, popular and full of life. He loved music, football and having fun with friends, and he planned to study International Business at university.
“But in May 2020, just before his 17th birthday, he began to complain of headaches. We also noticed he was dragging his right foot.
He was immediately sent to hospital
“We knew this wasn’t right and took him to the GP. He was immediately sent to hospital where he had a CT scan, and that night, we were told a mass had been found on his brainstem.
“A further MRI scan revealed a 5cm tumour and doctors suggested Daniel undergo a biopsy. The risks were explained to us, but we all agreed it was necessary.
“Afterwards, Daniel’s mobility declined and his motor skills were badly affected. But he was able to come home while we waited for the results.
It was the worst possible diagnosis
“Returning to hospital the following week, we were told Daniel had an aggressive brain tumour called diffuse midline glioma, or DMG, a terminal brainstem tumour mostly affecting children. It’s also known as DIPG.
“We had spent the week researching brain tumours so were aware we were being given the worst possible diagnosis. But when we asked about treatment options, it was hard to believe there weren’t any.
“Daniel started palliative radiotherapy, with the intention of slowing the tumour’s growth. But we felt a sense of hopelessness from the moment he was diagnosed. We knew he was dying.
“Daniel was vibrant, popular and full of life. He loved music, football and having fun with friends.”
During his illness he was the bravest boy
“We secured experimental drugs from overseas and Daniel was accepted on a clinical trial, but his cancer progressed so quickly he couldn’t take part.
“During his illness he was the bravest boy. He was so positive and didn’t like to think too deeply about what was happening. In his last three months, he could not get up, so we had a hospital bed installed in our bedroom.
“Daniel wanted us to care for him at home. A nurse came to administer morphine, steroids and anti-seizure medication, but we looked after him.
“He died on 30 November 2020, seven months after his diagnosis.
He wanted to raise money for research
“Daniel always hoped he would get better but understood the odds were against it. He wanted to raise money for brain tumour research, particularly for his type of tumour, to give others the chance of treatment he didn’t have.
“So, to keep his memory alive and honour his wishes, we set up the Doing it for Daniel Foundation. Initially, our aim was to provide gifts for children who had been diagnosed with cancer. Daniel loved the beach, so we also bought a beachside property so children with cancer and their families could have some respite by the sea.
We want to see new treatment options
“However, we also wanted to focus on research. Our hope is that children diagnosed with Daniel’s type of cancer could have a treatment option that would give them a chance and, if it could not save them, a decent quality of life for the time they have left. We want to see a time when a DIPG diagnosis is not a death sentence.
“We had followed Professor Chris Jones’ work in this field for some time and wanted to make a contribution to his research. We are proud to have achieved this and hope it will make a difference, so no other family will have to go through what we have experienced.”
Cancer discovery news
Our researchers are making the discoveries that defeat cancer. Read the latest findings from our world-leading research.