Timeline: How the ICR has led the way in myeloma research
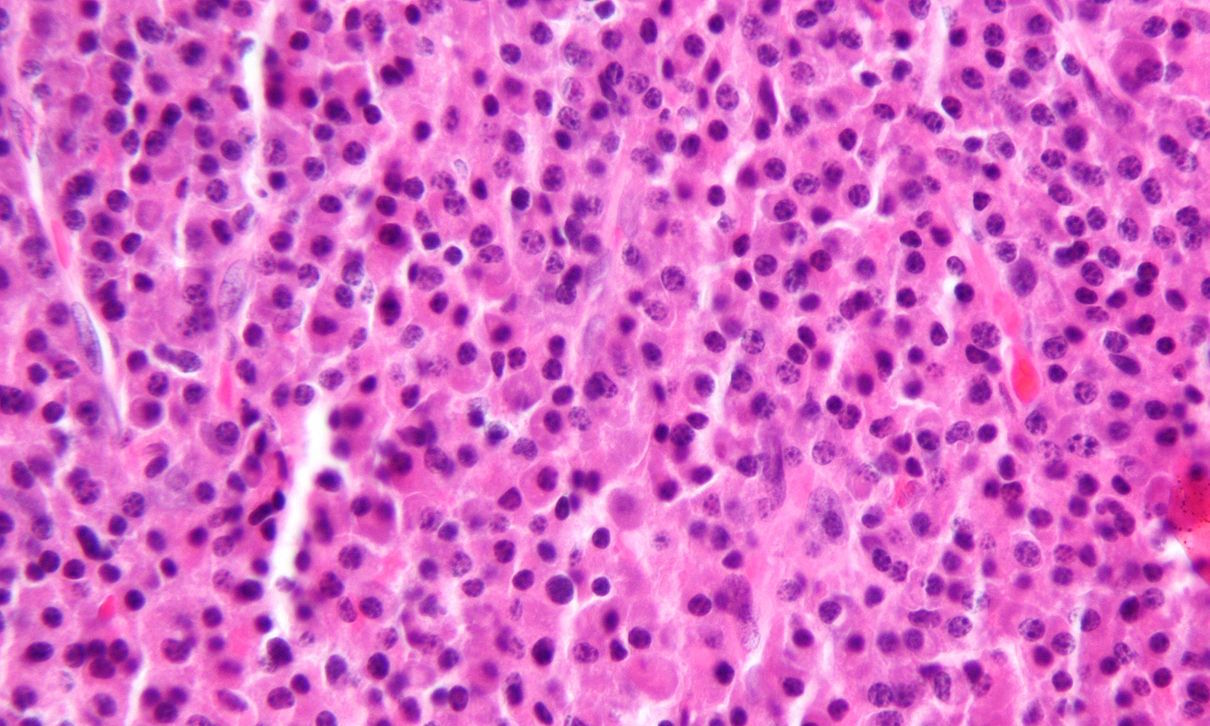
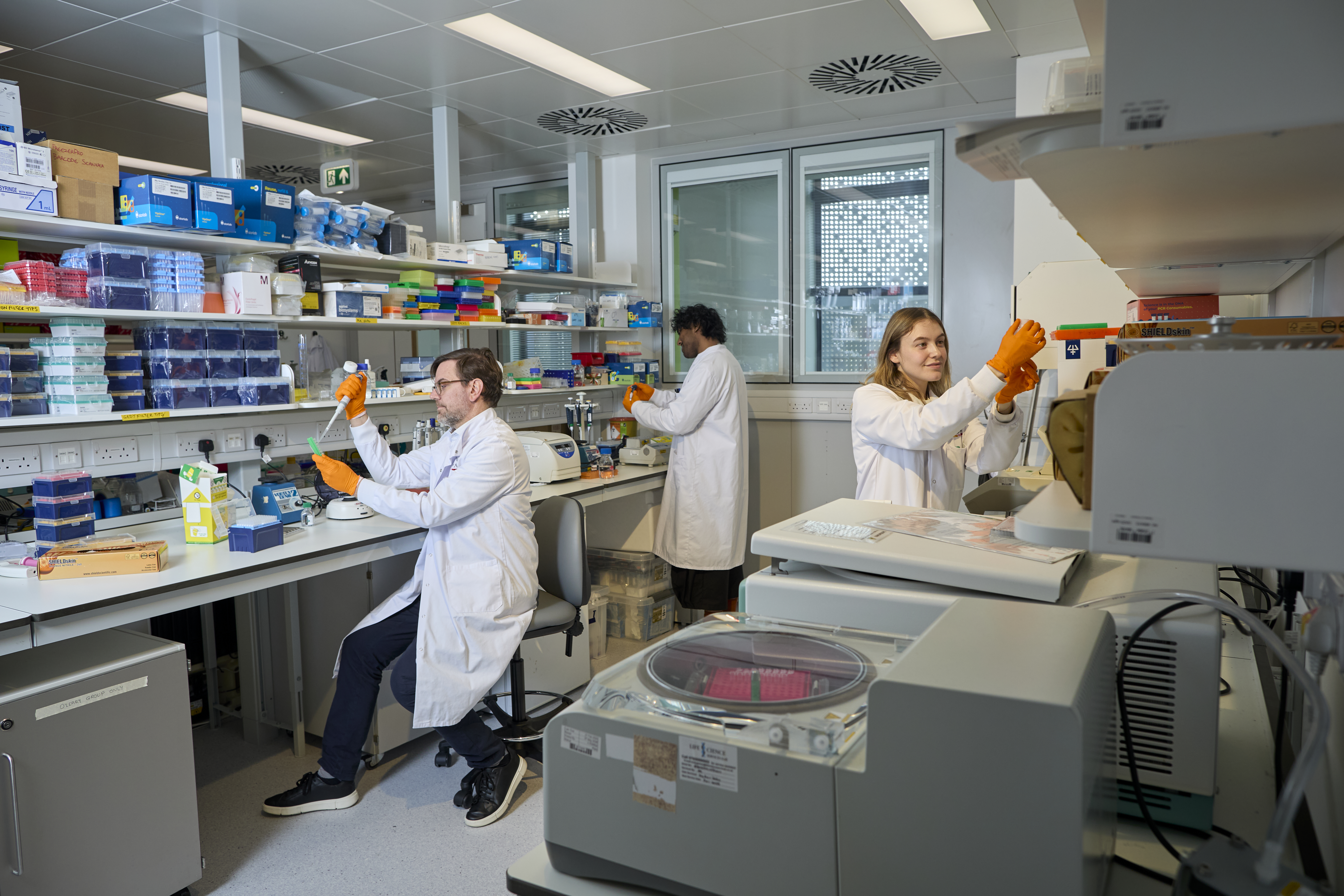
The Institute of Cancer Research (ICR) has been at the forefront of myeloma research for decades, with our scientists conducting innovative studies and clinical trials to better understand and manage this blood cancer.

2000s
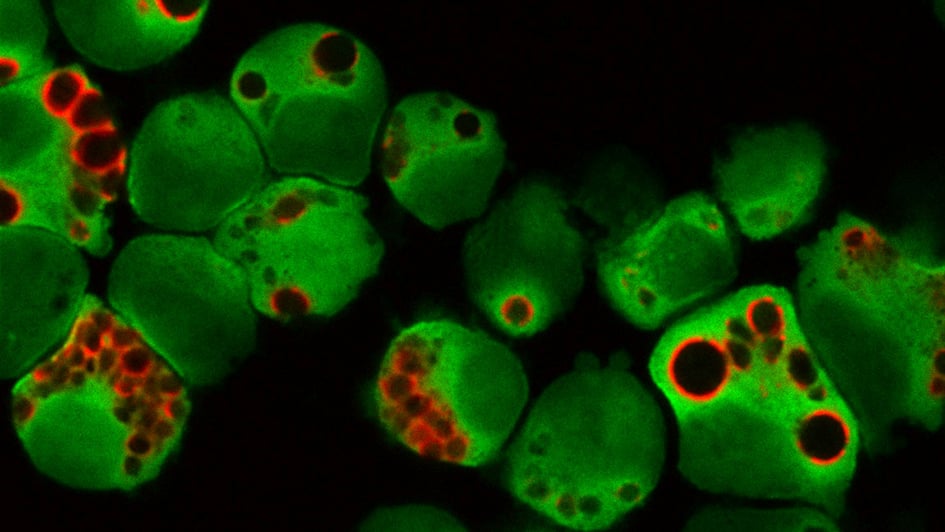
- In 2007, researchers in the ICR discovered the drug pictilisib, in collaboration with Genentech. It works by targeting the PI3K (phosphoinositide 3-kinase) signalling pathway, which is frequently altered in cancer cells. Preclinical studies have suggested that pictilisib could inhibit myeloma cell growth, but further clinical trials are required.
.jpg?sfvrsn=eb2d940b_1)
2010s
- The 2013 Medical Research Council Myeloma IX study, led by the ICR, found that adding a second drug to standard chemotherapy treatment can help patients with multiple myeloma live longer. The clinical trial results were published in Clinical Cancer Research.
- In 2013, an ICR-led study, published in the British Journal of Haematology, used genome sequencing to analyse patient samples from patients enrolled in the Medical Research Council’s Myeloma IX study. Researchers identified distinct microRNA signatures linked to myeloma risk, revealing a previously unrecognised ‘intermediate’ group of patients that may require urgent treatment.
- In 2013, ICR researchers found that analysing chemical changes in four key genes could provide a valuable tool for doctors assessing prognosis and designing personalised treatments for myeloma.
- In 2013, ICR scientists found that thalidomide could improve survival rates among myeloma patients with a low risk of recurrence. The study was published in the Journal of Clinical Oncology.
- In 2013, the ICR and Cancer Research Technology, the commercial arm of Cancer Research UK, announced a collaboration with Johnson & Johnson Innovative Medicine (formerly Janssen Biotech) to discover a potential new multiple myeloma drug targeting the unfolded protein response pathway. This pathway helps cells deal with stress caused by unfolded or misfolded proteins – where they fail to achieve their correct structure, causing cellular stress – and if this stress cannot be corrected, the cells succumb, which can be used in cancer treatment to eliminate them.
- In 2015, Professor Christina Messiou pioneered the use of whole-body diffusion-weighted MRI for patients with myeloma. This advanced imaging technique has improved disease diagnosis and monitoring. The research was published in the British Journal of Haematology.
- In 2016, researchers co-led by Professor Richard Houlston, Professor of Molecular and Population Genetics at the ICR and the Head of Division of the Cancer Genomics Group, identified a change in the DNA of patients with myeloma that increases their risk of developing myeloma bone disease, a common and serious complication of this cancer. The study, published in Leukemia, provided the first evidence that the development of myeloma bone disease is influenced by a patient’s DNA, which has implications for how patients are treated.
- In 2016, Professor Houlston identified eight new genetic variations in the human genome that could be linked to an increased risk of developing myeloma, building on existing evidence that myeloma can run in families. The research, published in Nature Communications, suggested these variants may subtly disrupt key genes involved in plasma cell development, increasing the likelihood of developing myeloma.
- In 2016, researchers at the ICR identified a mechanism that seemed to explain how a key genetic variant acts to increase the risk of developing myeloma. The study, published in Nature Communications, provided a new perspective on a protein pathway that increases myeloma risk even with slight disruptions. In doing so, it opened a new avenue of research into potential treatment approaches.
- In 2017, ICR researchers discovered that a certain gene, EZH2, is overactive in some cases of myeloma and associated with more aggressive forms of the disease. The research, published in Blood Cancer Journal, showed that people with high EZH2 expression levels did not live as long as patients with lower levels. They were also less likely to continue to respond to treatment.
- 2017 saw the launch of an ongoing phase II clinical trial called the MUK nine trial (OPTIMUM), which aims to improve outcomes for the 20 per cent of myeloma patients with high-risk disease, who generally have a worse outlook than other patients. The study, whose chief investigator is Professor Martin Kaiser, is using a stratified medicine approach – tailoring treatments to specific patient groups based on their individual characteristics and responses to therapy – and has incorporated genetic tests as a way to identify these groups of patients.
- In 2018, Professor Houlston identified six new DNA regions that, when altered, are linked to a higher risk of multiple myeloma. Alongside previously identified areas of the genome, these six new findings explain part of the inherited risk of myeloma. The people classed as highest risk, based on the genetic information, were identified as being three times more likely to develop the disease as the average individual. The research was published in Nature Communications.
- In 2018, researchers led by Professor Houlston and Professor Kaiser revealed 40 genes involved in the development of myeloma, increasing the understanding of the complex genetics behind it and helping drive the development of personalised medications. The research was published in Leukemia.
2020s
- In 2020, researchers at the ICR studied 329 patients across UK hospitals from the phase III Cancer Research UK Myeloma XI trial to understand the genetic patterns of multiple myeloma patients. Researchers developed a genetic test – looking at abnormal gene activity and genetic mutations – to identify certain patients who are at ‘ultra-high risk’ of their cancer progressing aggressively early on. The research was published in Leukemia.
- In 2023, researchers at the ICR and the University of Leeds announced promising results showing that a combination of five existing drugs – all individually licensed and in clinical use – can keep ultra high-risk myeloma at bay for longer. The research was published in the Journal of Clinical Oncology.

“I wake up every morning feeling grateful to be here.”
Julius Manyoni (pictured) is a Black Belt 6th Dan karate instructor. Having been fit and healthy all his life, he was shocked to be diagnosed with myeloma six years ago at the age of 60. Julius started chemotherapy, followed by a stem cell transplant, but these treatments didn’t work. He was then offered a targeted treatment which he’s been taking ever since. Julius is now in remission.
Your support helps
Everyone deserves the reassurance that effective treatment options will be available if their cancer returns. A regular gift from you will help our researchers stay one step ahead, giving more patients a better chance of living well with the disease. Help us discover a new generation of smart and targeted cancer treatments, so more people can survive blood cancer.