Radiotheranostics is an exciting new field that has the potential to transform how cancers are detected and treated. Robbie Lockyer finds out more.
Radiotheranostics, a groundbreaking approach that combines diagnostic imaging with targeted radiotherapy, is transforming cancer care by allowing clinicians to identify cancerous tissue, determine a patient’s suitability for certain therapies and deliver precise radiation directly to tumours. Central to this are site-specific or targeted radiopharmaceuticals – drugs that can both pinpoint and attack cancer, making them invaluable in cancer imaging and therapy.
Dr Kathy Chung Ying Chan, who recently joined The Institute of Cancer Research, London, as Group Leader of the newly formed Experimental and Translational Theranostics Group, which sits within the Division of Radiotherapy and Imaging, is developing novel radiotheranostics to actively find new ways to both diagnose and treat cancer.
Dr Chan’s research focuses on designing and synthesising radiopharmaceuticals that deliver both diagnostic and therapeutic radioisotopes – radioactive atoms used in medical imaging and cancer treatment – directly to cancer cells. It is also exploring how they can target different cancer types, such as breast, pancreas and prostate.
The world of radiotheranostics
Radiotheranostics refers to the use of radiopharmaceuticals for both imaging and treatment. These specialised compounds contain a radioisotope, along with a site-specific targeting molecule that directs it to cancer cells.
The radiopharmaceutical is injected intravenously into a patient and travels through the body, accumulating in the tumour. This allows clinicians to use diagnostic imaging techniques, such as position emission tomography (PET) or single-photon emission computed tomography (SPECT) scans, to see how much of the radiopharmaceutical is taken up by the tumour, assess whether the treatment target is present in the cancer cells and track how the tumour responds to therapy over time.
Upon switching to the therapeutic radioisotope, radiation can be delivered to selectively destroy the cancer cells, while minimising damage to surrounding healthy tissue.
Dr Chan said: “This is an exciting, rapidly emerging field. Essentially, these radiopharmaceuticals allow clinicians to see what they treat and treat what they see.”
Building a career in radiotheranostics
Dr Chan gained her PhD from La Trobe University in Australia, where she focused on synthetic chemistry for radiopharmaceutical applications. Developing SPECT imaging agents for Alzheimer’s disease allowed her to explore the intersection between chemistry and medical imaging.
Dr Chan said: “From early on in my career, I was fascinated by the idea of ‘building molecules’. It’s like assembling LEGO but with real-world applications. The compounds I developed during my PhD had dual functionality – they were fluorescent for optical fluorescence imaging and also could bind to radiometals for SPECT imaging. This sparked my long-term interest in developing new radiopharmaceuticals.”
Following her PhD, Dr Chan held a post-doctoral position at the University of Hong Kong, where she designed and developed fluorescent probes for small biomolecules detection, enabling the visualisation of specific processes inside cells in real time. Then, she joined the University of Oxford as a postdoctoral researcher to further expand her knowledge and experience in radiopharmaceutical development.
Developing KK02
During her time in Oxford, Dr Chan developed a library of targeted therapeutic compounds intended for use as radiotheranostic agents. The lead compound, KK02, is a promising candidate that binds specifically to cancer cells when combined with various diagnostic and therapeutic isotopes for imaging and/or therapy using radioactivity.
For instance, when KK02 is paired with the diagnostic radioisotope gallium-68 (68Ga) the resulting compound, 68Ga-KK02, enables whole-body imaging of therapeutic targets and the localisation of cancer cells. Once located, KK02 can be paired with the radioisotope lutetium-177 (177Lu), which delivers a targeted dose of radiation. In addition, the radiation of 177Lu-KK02 can be utilised for imaging, providing further confirmation of the radiopharmaceutical’s localisation, thus achieving real-time imaging.
These compounds, including KK02, were refined and patented by Dr Chan at the University of Oxford. However, driven by a passion to establish precision medicine through radiotheranostics and be a key figure in the field of nuclear medicine, she moved to the ICR to elevate her work and advance its development.
Dr Chan said: “The resource, expertise and collaborative environment at the ICR made it an ideal place to advance my research. Now, as a Group Leader, I have the opportunity to build a team and push the boundaries of radiotheranostics. Exploring new frontiers in cancer treatment and diagnosis will transform the future of targeted therapy and make a significant impact on patient care.”
Novel radiotheranostics in cancer therapy
Dr Chan’s primary project at the ICR revolves around developing and improving targeted therapeutic compounds to support radiotheranostics development, specifically for aggressive cancers.
Current development is focused on the lead compound KK02, which has shown promising results in binding to various radioisotopes, including 68Ga and 177Lu. Based on preliminary data with 68Ga-KK02 and 177Lu-KK02 in preclinical cancer models, Dr Chan observed a fast clearance from healthy tissue while effectively targeting tumours. Low radioactivity retention in healthy organs such as the kidneys, and the bloodstream, is a crucial characteristic of radiotherapeutic agents and reduces the risk of damage and complications for patients, improving the overall safety and effectiveness of the treatment.
Dr Chan said: “My team is exploring how it can be applied in various cancers such as prostate, pancreatic and breast cancer, as these cancers are aggressive when diagnosed, tend to spread and can be challenging to treat. We hope to further validate the therapeutic effectiveness of 177Lu-KK02 in upcoming studies, which we plan to publish before the end of the year.”
Her team is also investigating whether 177Lu-KK02 can be used in combination with immunotherapy to enhance its effectiveness. Preliminary data suggests that after treatment with 177Lu-KK02, there is a significant delay in tumour growth along with an increase in immune response inside the tumours, which could mean that solid tumours become more susceptible to immunotherapy.
Dr Chan said: “This is a field we’re very excited about as investigating combination treatment strategies could be key to improving outcomes for hard-to-treat cancers that are less responsive to radiotherapy or immunotherapy alone.”
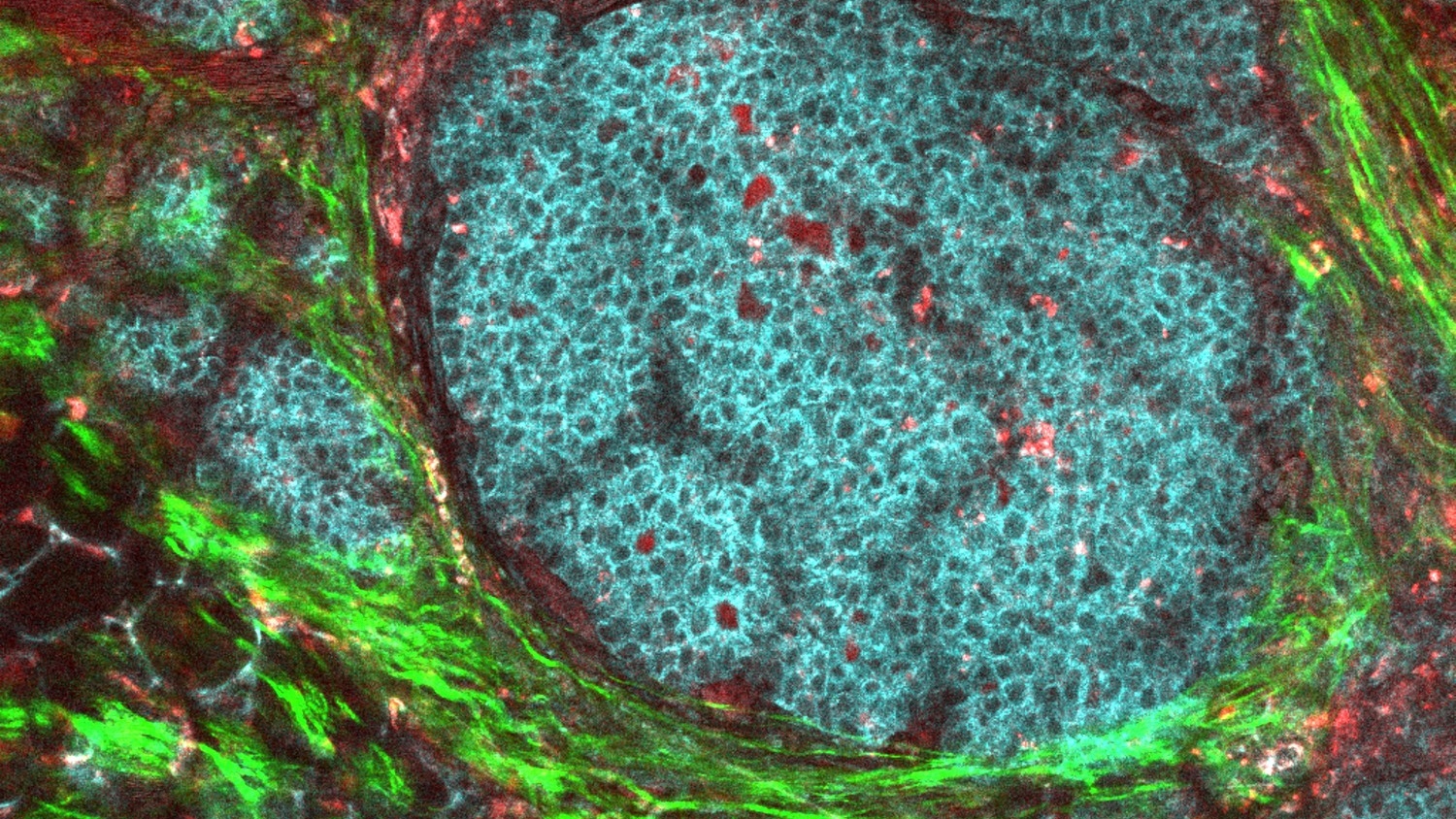
Image: Breast Tumour Microenvironment by The National Cancer Institute
KK02: profound real-world impacts
Dr Chan said: “One of the significant advantages of targeted radiopharmaceuticals is their global precision. Unlike traditional chemotherapy or external beam radiotherapy, radiopharmaceuticals can selectively target tumours in the body with minimal side effects. This opens the door for personalised medicine – tailoring treatments based on a patient’s specific tumour biology, even in metastatic cancer, to improve treatment outcomes.”
“The radiopharmaceutical I have developed has great potential to treat cancer patients and could possibly be used more broadly due to its target being expressed in many different cancer types. With more funding, I can undertake further research and collect more data to move this forwards.”
Not without challenges
Despite radiopharmaceuticals’ exciting potential, challenges remain. One major hurdle is ensuring that they do not accumulate in healthy tissues, leading to unwanted toxicity. Dr Chan’s research team is focusing on refining radiopharmaceutical scaffolds – the structural frameworks that carry radioactive compounds – with faster clearance from healthy tissues while maintaining high tumour retention.
One common misconception is that radiopharmaceuticals, and radiotherapy treatment more broadly, are inherently toxic due to their radioactive nature. In reality, these therapies are designed to be highly targeted, delivering radiation precisely to where it’s needed while sparing healthy tissue.
Beyond the scientific challenges, regulatory approval and accessibility remain significant hurdles due to radiopharmaceuticals’ relative newness and intricate nature. These treatments require rigorous testing, and their production at scale can be complex and expensive.
Dr Chan said: “As more clinical trials demonstrate radiopharmaceuticals’ effectiveness, I believe we will see increased adoption in mainstream oncology.”
The road ahead
Beyond Dr Chan’s work, the ICR is contributing to the development of radiotheranostics for different cancer types. Dr Sally George, Group Leader in Development Oncology and Paediatric Oncology and Consultant Paediatric Oncologist at The Royal Marsden NHS Foundation Trust, was a co-author on a research paper detailing radiotheranostics for neuroblastoma, which was published in The Journal of Nuclear Medicine this year.
Dr George is looking at how radiotheranostics can be used in neuroblastoma, where it has potential due to the cancer cells having unique biological features – such as specific chemical signals and cell membrane surface markers – that are different from those found in most healthy tissues.
The paper outlined promising strategies to enhance radiotheranostics for neuroblastoma, such as improving the specificity and efficacy of radiopharmaceuticals. However, it also highlighted key challenges, including the need for extensive clinical trials to bring these therapies to wider use.
Dr George said: “Radiotheranostics presents an exciting opportunity to refine treatment strategies for neuroblastoma. By continuing to improve how these therapies are developed and delivered, we can work towards making them a viable option for more patients in the future.”
These challenges are similar to those faced in Dr Chan’s projects involving her developed radiotheranostics, underscoring the broader difficulties in bringing radiotheranostics to clinical practice. Yet, with continued innovation and collaboration, the field is making strides toward more precise and effective cancer therapies.
Dr Chan said: “This is just the beginning. We are only scratching the surface of what’s possible with radiotheranostics, and I’m excited to see how this field evolves over the next decade.”
Header image: Dr Kathy Chung Ying Chan