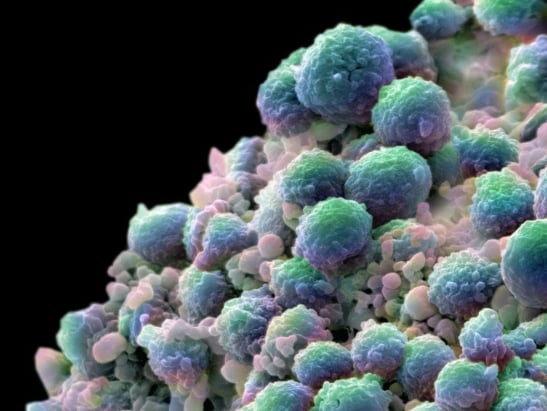
Image: A colour-enhanced image showing a clump of prostate cancer cells
At the ICR, we are interested in how to make cancer treatments kinder and more practical for patients. With prostate cancer being the most common cancer in men in the UK and many other countries, and with more than 47,500 new UK cases and almost 12,000 deaths annually, there remains a need to improve our understanding of how to deliver treatment schedules to make them more effective and convenient.
Our researchers have been central in conducting research in this area that has underpinned new standards of care for prostate cancer, leading to substantial benefits for both patients and healthcare systems across the world.
Prostate cancer radiotherapy
In general, radiotherapy and surgery are considered the most effective treatment options for cancer, with around 30 per cent of men with prostate cancer receiving radiotherapy as their main treatment. Side effects for most patients tend to be fleeting, but there is the risk of developing more serious problems such as bladder or bowel damage after treatment.
Tony Herbert, who was diagnosed with prostate cancer in 2018, said: “My radiotherapy treatment was quite intense. I had 37 sessions, which took place over seven weeks. It was wearing travelling to the hospital every day for such a long time, so it would be great if the time could have been reduced – the shorter, the better!”
New ways of targeting tumours more precisely have helped increase the effectiveness of radiotherapy – increasing the dose that can safely be given while minimising damage to surrounding tissues. Intensity modulated radiotherapy (IMRT) – pioneered at the ICR – is one such approach which has improved outcomes and quality of life for many men with prostate cancer.
IMRT is a type of external-beam ‘conformal’ radiotherapy which shapes the radiation beam to match the contours of the tumour, delivering higher doses to target areas of the prostate while avoiding healthy organs and tissues. Medical physicist Professor Steve Webb was central to the development of IMRT, through his own research and co-head of the Joint Department of Physics at the ICR and our partner hospital, The Royal Marsden NHS Foundation Trust, from 1998 to 2011.
Higher doses in smaller numbers
IMRT has provided a more dynamic, precise and technologically advanced treatment option for men with prostate cancer – and it has paved the way for developing streamlined treatment regimens to reduce the burden on patients, as well as on healthcare systems.
Early on, our researchers recognised that the answer to more effective radiotherapy might lie with finding the best possible radiation dosage, or ‘fractionation’. Evidence from ICR research and wider studies pointed to the idea of delivering smaller, higher doses of radiotherapy – an approach called hypofractionation, which might be able to reduce treatment toxicity without compromising cancer control.
There were also major advantages to both patients and healthcare systems in finding ways to reduce the number of hospital visits required for a course of radiotherapy.
Lessons from breast cancer treatment
Before our practice-changing research in prostate cancer radiotherapy, ICR researchers including Professor Judith Bliss and Professor John Yarnold had already showed that hypofractionated radiotherapy had advantages for women with breast cancer without increasing side effects.
Early studies suggested that prostate cancer, too, might be more sensitive to larger fractions than smaller ones. Giving treatment in a smaller number of fractions also had the potential to increase the resource efficiency of IMRT by reducing the number of times treatments had to be given.
By the early 2000s, our researchers were keen to explore whether a switch to using hypofractionated IMRT for prostate cancer could have benefits for both patient safety and for the efficiency of care.
Professor David Dearnaley, who headed the ICR’s Clinical Academic Radiotherapy Team before his retirement in 2020, says:
“IMRT used to be more costly because of long treatment times, and at the time it wasn’t yet funded as a prostate cancer treatment. Based on previous literature, it seemed that hypofractionation with IMRT could help to remedy both of these issues. My belief was that the change of technology to using IMRT was going to have a greater benefit on patients by reducing side effects than the effect of any risk from decreasing the number of fractions.”
The REF is the UK’s system for the assessment of research quality and impact at its higher education institutions. To mark our outstanding success, we are celebrating some of the ICR research programmes that have been changing the lives of cancer patients.
Read more about REF2021
Hypofractionation in the clinic
Professor Dearnaley led a UK-wide trial that established the effectiveness of high-dose conformal radiotherapy for prostate cancer – finding that the radiotherapy dose could be safely escalated to 74 Gray (Gy) in 37 fractions, or doses, reducing side effects without compromising on patient outcomes. This research led to the recommendation by the NHS England Clinical Commissioning Policy in 2014 that the dose regimen for prostate cancer should be changed.
It also helped kickstart the largest radiotherapy study in localised prostate cancer to date: the Conventional or Hypofractionated High-dose intensity modulated radiotherapy in Prostate cancer, or CHHiP, trial. Coordinated by the ICR’s Clinical Trials and Statistics Unit (ICR-CTSU) and led by Professor Dearnaley and Professor Emma Hall, Deputy Director of the ICR-CTSU, the CHHiP trial set out to compare the effectiveness of a shorter, hypofractionated radiotherapy regimen with the recommended regimen of 74 Gy.
CHHiP recruited more than 3,200 men with localised prostate cancer, enrolled from 71 centres, to receive IMRT. Patients were randomly assigned to either the standard radiotherapy regimen of 74 Gy delivered in 37 fractions over around seven weeks, or one of two new hypofractionated regimens: 60 Gy in 20 fractions or 57 Gy in 19 fractions, over an average of four weeks.
One of the trial’s central questions was whether hypofractionated radiotherapy would provide the same therapeutic benefit for patients without increasing side effects. In 2012, the phase I and II results showed that the 60 Gy in 20 fractions schedule was just as well tolerated as the standard treatment, with no difference in side effects.
Importantly, the phase III findings established in 2016 that hypofractionation of 60 Gy in 20 fractions was not inferior to the standard regimen for treating patients’ cancer. The biochemical or clinical failure free survival at five years was 88.3 per cent in the 74 Gy control group, 90.6 per cent in the 60 Gy group and 85.9 per cent in the 57 Gy group.
As Professor Dearnaley explains: “We really wanted to do a trial where centres were able to use IMRT to treat prostate cancer patients, and provide a way to allow more centres to get on the IMRT pathway, since a lot of training is needed to implement it.
“The CHHiP trial really facilitated the introduction of this type of radiotherapy and its wider adoption as a prostate cancer treatment.”
Fewer hospital visits
Hypofractionating radiotherapy meant that patients could make fewer hospital visits, in turn entailing a better use of radiotherapy resources and a more convenient treatment schedule. Instead of an average of 37 visits, the occasions that patients needed to visit hospital or treatment centres could be cut down to 20 – amounting to around 238,000 hours saved a year in travel time.
The change was popular with patients: five-year patient-reported outcomes of the trial published in 2021 showed that people considered the hypofractionated treatment to be equally as favourable as the norm.
“People were very attracted to the idea of a shorter treatment, cutting it down from almost eight weeks to just four. We found that virtually all were enthusiastic about participating in the trial, which helped the recruitment process considerably, especially because we needed to recruit such large numbers,” says Professor Dearnaley.
Aside from the main trial analysis, an exploratory analysis involved looking at the lower 57 Gy dosage in a subset of participants over the age of 75. This showed that 57 Gy in 19 fractions, despite failing to meet the non-inferiority criteria in the main trial report, was better tolerated in this group and didn’t cause many side effects – offering an appropriate treatment option for elderly patients.
The team also investigated the use of image-guided radiotherapy (IGRT) to further reduce side effects by more accurately targeting radiation at the cancer during treatment.
A new standard of care for prostate cancer
The benefits of the 60 Gy schedule, as demonstrated by CHHiP, helped to make a robust case for hypofractionated radiotherapy for treating localised prostate cancer. The trial overturned the conventional belief that keeping individual doses low was the optimal approach, establishing a new regimen that substantially reduced treatment costs and times, and helped to increase the efficiency of IMRT.
In the UK, NHS England recommended 60 Gy in 20 fractions as a safe and effective treatment for prostate cancer in 2017, establishing a new standard of care, with use of this regimen increasing by more than 40 per cent between 2012/13 and 2016/17.
The National Institute for Health and Care Excellence (NICE) agreed with the NHS recommendation as part of the update to its wider prostate cancer guideline. Hypofractionation using the 60 Gy in 20 fraction schedule has now become the new standard of care and in 2020 was used in 96 per cent of prostate cancer patients undergoing radiotherapy, as reported by the National Prostate Cancer Audit.
International change
The CHHiP trial also helped to propel change internationally. Several cancer societies in the US, including the American Society for Radiation Oncology (ASTRO) and American Society of Clinical Oncology (ASCO), supported the routine use of 60 Gy in 20 fractions in the clinic, concluding that the data was sufficiently robust to justify a new guideline.
International bodies such as the European Society for Radiotherapy and Oncology (ESTRO) and the Royal Australian and New Zealand College of Radiologists also endorsed this recommendation.
By implementing the CHHiP regimen nationwide, the NHS is estimated to save £28 million a year from reduced treatment fractions and hospital attendances, while US healthcare systems have the potential to save approximately $360 million in treatment costs.
The regimen can also help things along in the clinic from a practical standpoint. Prostate cancer currently accounts for around 28 per cent of the overall workload for radiotherapy treatments, but hypofractionation has increased the availability of radiotherapy resources for other purposes and reduced waiting times for patients.
The implications of CHHiP can also improve how current prostate cancer patients such as Tony Herbert receive their treatment. He said of his course of radiotherapy: “From time to time I have some bleeding, which is a result of the damage caused by the radiotherapy. If the radiotherapy could have been more targeted, and delivered more precisely, it would certainly have been to my benefit, so any research advances in this area are great news.”
Appetite for hypofractionation
With the wide uptake of the CHHiP regimen, our researchers are continuing to build on the success of the trial by exploring how hypofractionated radiotherapy can be delivered to provide an even greater therapeutic benefit for prostate cancer patients.
Currently, the ICR and The Royal Marsden are leading the international, multicentre PACE trial, the results of which are expected in 2023. The aim of PACE is to investigate whether hypofractionation using stereotactic body radiotherapy (SBRT), which involves directing radiation at the tumour from many different angles, could be a more effective treatment for prostate cancer than prostatectomy – surgery to remove the prostate – or conventional radiotherapy.
Professor Hall says: “The move to 20 fractions for prostate cancer radiotherapy has been widely taken up thanks to the results of the CHHiP trial, and the increased appetite for hypofractionation has been further evidenced by the strong recruitment to PACE.
“The PACE study will establish whether an even shorter radiotherapy treatment of five fractions – which some health centres have been pushing for, especially during Covid-19 – could also be an effective treatment regimen for prostate cancer. If successful, it has the potential to further improve patients’ quality of life and the efficiency of radiotherapy treatments.”
Getting the right balance between dosage and toxicity is paramount when it comes to hypofractionated radiotherapy. It is one that the CHHiP trial has successfully established for prostate cancer with the 60 Gy regimen – demonstrating the value of this approach and the significant effect it has had on remodelling prostate cancer treatment to reduce healthcare pressures and, most importantly, to improve patient’s lives.