In the early days of radiotherapy, it was generally thought that the biggest tolerated dose should be given as fast as possible.
It wasn’t until the 1920s that Professor Claude Regaud at the Radium Institute in Paris recognised that radiotherapy may be better tolerated and more effective if delivered more slowly with modest doses per day over several weeks.
The reason for splitting a radiation dose is to maximise the killing of cancer cells, while minimising damage to neighbouring healthy tissues. This approach, known as fractionation, is still one of the most important underlying principles in modern-day radiotherapy.
Fraction size sensitivity reflects the ability of the cell to repair lethal double-stranded DNA breaks caused by radiotherapy, prior to the next fraction of radiotherapy. All tumours are sensitive to the total radiation dose delivered, but not all are sensitive to the size of the fractions, or daily dose, used to deliver the total dose.
Since the majority of dose-limiting healthy tissues – such as skin, muscle and ribs – are consistently sensitive to fraction size, historical practice has been to spare them as much as possible using small (1.8–2.0 Gy (Gray)) fractions to deliver the highest possible total dose (60–90 Gy) to the cancer.
However, recent research lead by The Institute of Cancer Research, London and The Royal Marsden has shown that breast and prostate cancer are more sensitive to fraction size than previously thought, which means that using small fractions has no advantage when treating these cancers.
Discovering predictive markers
Dr Navita Somaiah is a Clinician Scientist at the ICR and a Clinical Oncology Consultant at The Royal Marsden studying mechanisms underlying fraction size sensitivity.
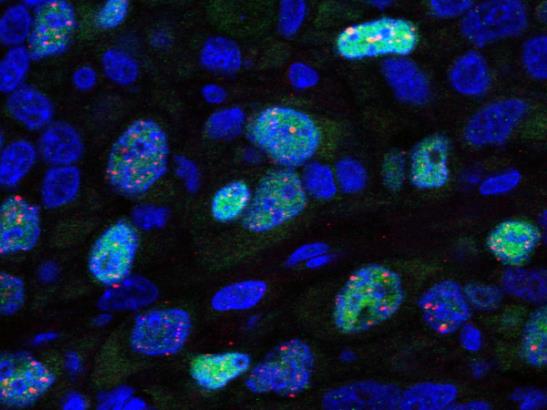
The focus of this research is on biomarkers – molecular and cellular measures – that can be used to indicate the sensitivity to fractionation treatment.
Dr Somaiah says: “Previous research shows that small fractions spare breast and prostate cancer as much as the surrounding normal tissues. Our research from the START breast cancer trials show that a lower total dose delivered in fewer, larger fractions – hypofractionation – is just as safe and effective as the standard treatment, which delivers a high total dose in 25 small daily doses.
“Given the evidence for variation in fraction size sensitivity between tumour types, it is also possible that significant variation in sensitivity exists within tumour types. That’s why we are looking for predictive biomarkers of sensitivity to fraction size that allow stratification of patients for treatment with the most appropriate fractionation regimen.”
The ICR, along with The Royal Marsden, is leading the START and CHHIP trials – the largest breast and prostate cancer hypofractionation trials in the world. Other national trials include the IMPORT and FAST Forward studies, which are soon expected to change NHS practice in the way hypofractionated radiotherapy is delivered to women with breast cancer.
“We are capitalising on our global lead in breast fractionation trials with an extensive translational radiobiology research programme running parallel to these trials,” explains Dr Somaiah. “Using banked tumour samples from these studies, we are working towards identifying biomarkers of radiation fraction size sensitivity and radiosensitivity.”
Personalised radiotherapy
A new collaboration between the breast and prostate teams is also allowing the identification and validation of biomarkers in two tumour types that share similar average sensitivities to daily doses of radiation.
“In addition to molecular pathology and genomic analysis, we are looking at cellular and molecular determinants of fraction size sensitivity with a newly established collaboration with the Genome Damage and Stability Centre in Sussex,” reveals Dr Somaiah.
Much like Regaud’s research carried out nearly a century ago, Dr Somaiah’s translational research is helping to shape the future of radiotherapy.
If we have more personalised radiotherapy based on biomarkers of fraction sensitivity, we can move away from the ‘one fraction size’ fits all approach that has been a feature of radiotherapy for decades.
Combined with our drive to develop more accurate imaging techniques and efforts to improve the effectiveness of radiation treatment, our radiotherapy research is already helping to make huge contributions in improving the outcome for patients undergoing radiotherapy.