Scientists have developed a new high-tech system for measuring the body’s immune response to cancer – as a way of assessing how rapidly the disease is likely to progress.
The system combines computerised imaging of tumour samples with statistical analysis, and is the first objective method to measure the interaction between a patient’s immune system and their tumour.
Details of the technique’s development are published today (Wednesday) in the Journal of The Royal Society Interface, in a research paper by scientists at The Institute of Cancer Research, London.
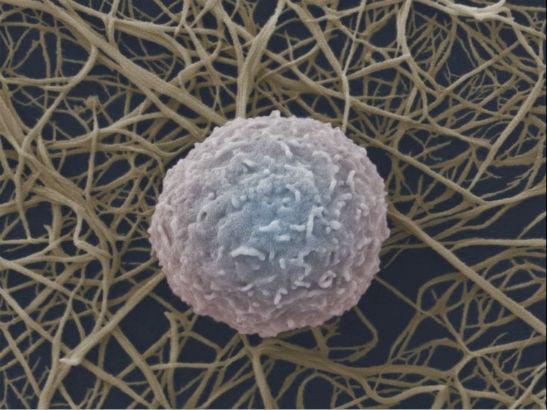
By measuring the type and number of lymphocytes – a type of white blood cell – in tumours, the test indicates the level of success the immune system is having at keeping a tumour in check.
It could complement existing labour-intensive methods of tumour sample analysis, helping doctors pick out tumours that are evading the immune system and may need the most intensive treatment.
The level of immune response to a tumour is known to have a significant effect on how likely it is to progress into an aggressive and fatal form. Tumour samples are currently assessed visually by pathologists for signs of immune infiltration – but this is a subjective test with limited accuracy.
In the study, scientists at The Institute of Cancer Research (ICR) analysed 181 samples from women with a type of breast cancer called triple-negative breast cancer.
They developed a system which split lymphocytes into three classes, depending on their location within the tumour, and calculated how many of each type were present in each sample, and how many cancer cells were present. Women in the study whose ratio of ‘intra-tumour’ lymphocytes to cancer cells was below a certain threshold were much more likely than average to die within five years.
Women with fewer than around eleven intra-tumour lymphocytes per 1,000 cancer cells had an average five-year survival rate of 49 per cent, compared with an average of 80 per cent in triple-negative breast cancer as a whole.
The study also found a correlation between immune infiltration of tumours and increased levels of a protein called CTLA4, suggesting it could be a potential treatment target in this breast cancer type. A cancer treatment targeting CTLA4, called ipilimumab, is already used in metastatic melanoma.
The study was led by Dr Yinyin Yuan, who works within the ICR’s Centre for Evolution and Cancer – established to understand how cancers adapt to their environment and a patient’s immune system, and how they evolve over time.
Dr Yinyin Yuan, Team Leader in Computational Pathology and Integrative Genomics at The Institute of Cancer Research, London, said:
“The most aggressive cancers often evolve ways to hide from the body’s immune system, protecting them from being seen and attacked by white blood cells. Pathologists do examine tumour samples under the microscope to assess immune response to a cancer – and this expertise can never be fully replaced – but there is currently no objective measure of immune response used in the clinic.
“Our test combines imaging technology with computerised analysis of large amounts of data from tumour samples – which typically contain more than 100,000 cells. We found the technique could accurately identify high-risk tumours that were evading the body’s immune system in this type of breast cancer, and hope it can be adapted and added to doctors’ arsenal against a variety of cancers.”
Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said:
“We’re increasingly becoming aware of the importance of the complex interaction between the tumour, immune system and surrounding environment for a patient’s prognosis and their response to treatment. This study is important in that it brings together different types of expertise – imaging, tumour biology and bioinformatics – to measure by computer the interaction between cancer and the immune system, and to assess what it means for patients.”