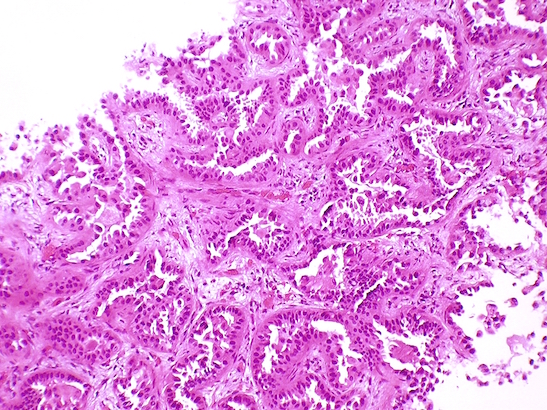
Adenocarcinoma with predominant lepidic growth pattern, image from Yale Rosen CC BY-SA 2.0
Scientists have shown that a drug combination slows cancer cell growth in a type of non-small cell lung cancer when tested in the lab, offering potential for developing new treatments in the future.
The drug combination delivers a double blow to the way the KRAS gene makes cancer cells grow, according to a Cancer Research UK-funded study.
KRAS is estimated to be mutated in 15 to 25 per cent of people with non-small cell lung adenocarcinomas[1] – a disease affecting around 10,400 people in England each year[2].
The study, by scientists at The Institute of Cancer Research, London, and The Institut Gustave Roussy in France, looked at whether blocking the functions of two proteins called MEK and m-TOR would stop or slow down the growth of non-small cell lung adenocarcinoma cells in the laboratory.
The two proteins are switched on by the KRAS gene, which helps control how and when the cells divide. When the gene is mutated cells divide uncontrollably and can develop into cancer.
The scientists used the drug trametinib to block MEK, and AZD2014 to block m-TOR[3].
They found that blocking m-TOR slowed cancer cell growth more than MEK. But using the MEK and m-TOR inhibitors together was better at stopping the cancer cell growth compared with either drug alone[4].
The study was published in the British Journal of Cancer.
Where current clinical trials concentrate on blocking MEK in KRAS-driven lung cancers, this research suggests this could be improved by adding m-TOR inhibitors.
Lead author, Dr Udai Banerji, Cancer Research UK Reader at the ICR said: “There aren’t yet any drugs to treat cancers with the KRAS mutation, so our study has given us a direction to focus future research on. We’re really delighted to have been able to get at the KRAS gene in laboratory conditions. This is still early work so we’ll need more years of research to test the drug combination – checking that it’s safe for patients and finding the right dose – before it could be used routinely in the clinic.”
Nell Barrie, Cancer Research UK’s senior science information manager, said: “Lung cancer is the biggest cancer killer in the UK, partly because it tends to be diagnosed at a late stage when it’s already spread. Only seven per cent of people diagnosed with lung cancer survive their disease for ten years or more, and this is why Cancer Research UK is prioritising investment into lung cancer research to save more lives from this disease.”
[1] C. Lovly, L. Horn, W. Pao. 2015. KRAS in Non-Small Cell Lung Cancer (NSCLC). My Cancer Genome https://www.mycancergenome.org/content/disease/lung-cancer/kras/
[2] Calculated by the Statistical Information Team at Cancer Research UK based on the annual average number of adenocarcinoma (ICDO3 M814-M838, behaviour code 3 only) cases of lung cancer (ICD10 C33-C34) diagnosed between 2011-2013 in England. Please note that there may be further cases of lung cancer that have not been classified with the appropriate morphology coding within this dataset, therefore this figure could be an underestimate.
[3] The drug AZD2014 is experimental and still in clinical trials to treat solid tumours (all cancer types except leukaemia, lymphoma or myeloma). Trametinib has been licensed for use in the UK in combination with dabrafenib to treat metastatic melanoma in adults with a BRAF mutation.
[4] The m-TOR inhibitor reduced growth by more than half (52 per cent), while the MEK inhibitor slows growth in almost a fifth of cells (18 per cent). The two drugs used together slow growth by around four-fifths (79 per cent) when compared to normal NSCLC cells.