A combination treatment of immunotherapy with the experimental drug guadecitabine may reverse a cancer’s resistance to immunotherapy – making it sensitive to treatment again, a new study has found.
Overall, 37 per cent of cancer patients enrolled in the trial had their disease kept in check for 24-weeks or more after receiving the immunotherapy drug pembrolizumab with guadecitabine – with signals that the immune system was being activated within the tumours of some, especially those with non-small cell lung cancer (NSCLC) that had previously progressed on pembrolizumab.
This combination treatment could be a new option for patients with lung cancer and other tumours whose cancer has progressed and resisted immunotherapy.
Pembrolizumab is an immune checkpoint inhibitor drug that has been successful at treating a range of solid tumours, including those of NSCLC and melanoma. However, cancers can develop resistance to pembrolizumab and some patients who initially benefit from the drug will eventually see their disease progress.
Overcoming drug resistance
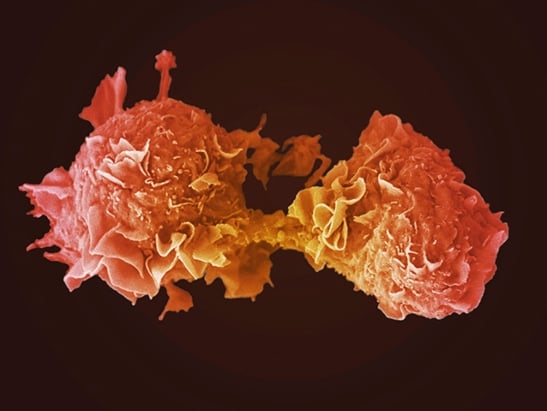
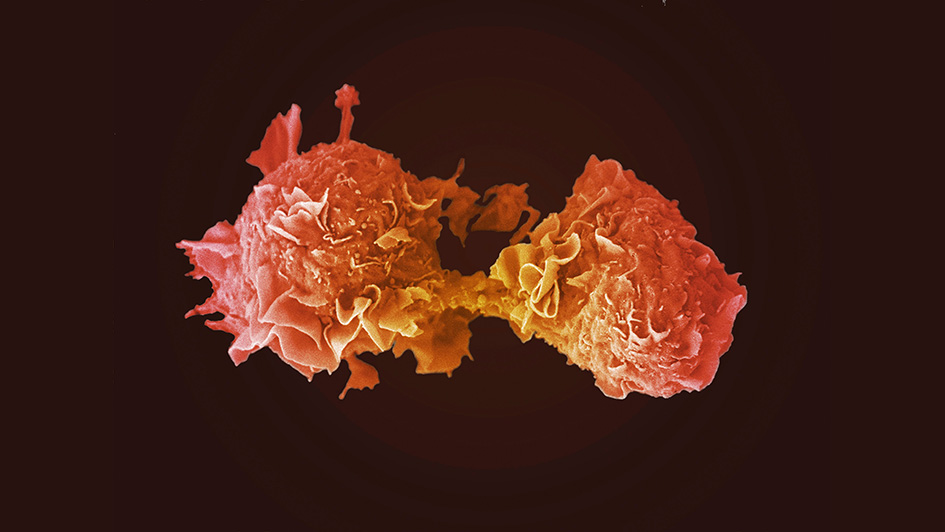
Guadecitabine may be able to help overcome this resistance because it is a DNA hypomethylating agent, which means it works by removing methyl groups from DNA. Methylation of cancer DNA is thought to play a role in cancer’s ability to suppress the immune system and therefore evade the action of immune checkpoint inhibitor drugs.
Clinical research led by researchers at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust aimed to investigate whether guadecitabine had the potential to overcome resistance to pembrolizumab in a combination approach and establish the dose and side effects of this treatment.
The study used a combination of guadecitabine and pembrolizumab to treat 34 patients with cancer that included those with lung, breast and prostate cancer, 30 of whom had their cancer analysed for immune activity and cancer growth. Every three weeks, patients received guadecitabine on the first four days of treatment and pembrolizumab on the first day only over the course of the three-year trial.
This work is one of the first studies to look at a guadecitabine-pembrolizumab cancer drug combination with immunological measurements. It was published in the Journal for Immunotherapy of Cancer. Guadecitabine was supplied by Astex Pharmaceuticals, Inc. and the study received funding from MSD, with support from a grant from Cancer Research UK and the Experimental Cancer Medicine Centre Initiative.
Beneficial for NSCLC patients
Of the 30 patients who had their cancer activity analysed, 37 per cent had their disease controlled and did not see it worsen for 24 or more weeks from the guadecitabine-pembrolizumab combination.
60 per cent of the cohort had previously received immune checkpoint inhibitor therapy, 47 per cent of whom had seen their cancer progress after treatment. After the combination treatment, 39 per cent of patients’ cancer did not get worse after 24 weeks – highlighting the potential of this approach for when immune inhibitors on their own may have failed.
The combination treatment seemed to be particularly beneficial for NSCLC patients; 42 per cent had their disease controlled for 24 weeks or more, including patients whose cancer had previously progressed on immune checkpoint inhibitor therapy – a sign that the immune system may be being restimulated against the tumour.In addition, the study established a safe dosage of guadecitabine with pembrolizumab and found that the treatment had tolerable side effects.
The researchers also took tumour and blood samples to show that immune activation was taking place in some patients’ tumours. For example, some patients had significant increases in certain immune cells, such as white blood cells, as well as changes in immune cells circulating in the blood stream.
Samples from 15 patients also showed that demethylation had occurred in tumours after treatment, while RNA analysis confirmed that inflammation was taking place in the tumour that wasn’t present before the combination was given.
Targeting cancer after it stops responding to immunotherapy
Study lead Dr Anna Minchom, NIHR BRC Clinical Scientist in the Drug Development Unit at The Institute of Cancer Research, London and a Consultant Medical Oncologist at The Royal Marsden NHS Foundation Trust, said:
“Immunotherapy has shown amazing promise in cancer care over the last decade, but it doesn’t work well in all cancers and cancers can often become resistant. It was interesting to explore the guadecitabine-pembrolizumab combination in this study as it could have the ability to reverse a cancer’s resistance to immunotherapy and potentially benefit a large number of patients.
“We have demonstrated it might help those with non-small cell lung cancer, for example, who have few treatment options if chemotherapy and immunotherapy stop working for them. This combination might be a way to target their cancer even after it has stopped responding to immunotherapy.”
Guadecitabine and pembrolizumab could offer promise
Study Chief Investigator Professor Johann de Bono, Professor of Experimental Cancer Medicine at The Institute of Cancer Research, London and Consultant Medical Oncologist at The Royal Marsden, said:
“I think one of the most important things about this trial is that we used multiple different methods to look for changes in the immune system, robustly showing that it was being influenced by the combination treatment.
“In the long term we hope that if these effects are confirmed in other patient groups and future studies, guadecitabine and pembrolizumab could help to tackle some of the resistance to immunotherapy we see in too many types of cancer.”
'I am off pembrolizumab and have no cancer in my body'
Alison Sowden, 61, from Dorset, was diagnosed with non-small cell lung cancer in 2018. She said:
“In October 2018, I found a tiny lump in my neck and my GP referred me to the ear, nose and throat department at my local hospital. After various scans, a biopsy and an ultrasound, I was told I had cancer, which had actually started in my lungs. Then I was told that I had a year left to live.
“An amazing consultant referred me for the immunotherapy drug pembrolizumab. I was on pembrolizumab alongside chemotherapy until November 2021. Three years after being diagnosed, I am off pembrolizumab and have no cancer in my body. Pembrolizumab has given me years of life that I thought I’d never get to experience, and I’m incredibly grateful.
“Like many other people out there, I know there is a chance that my cancer may come back and develop resistance to treatment, so it is reassuring to know research efforts aiming to reverse cancer’s resistance to immunotherapy are underway. I hope this new experimental drug combination will eventually make it to the clinic and help people who have developed resistance to pembrolizumab.”
Cancer can adapt and evolve to evade treatment. We are looking for new ways to stay one-step-ahead of cancer and using treatments in combination is one way of doing this. Support our research today to unlock new combination therapies, and help more people survive cancer.
Let’s finish cancer, together.