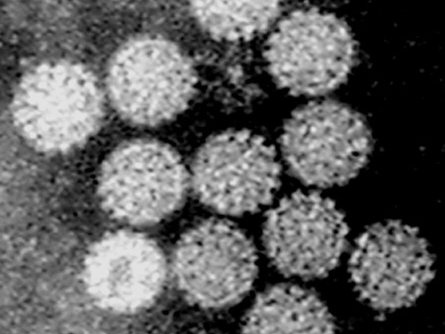
Image: Electron microscope image of Papilloma virus. Credit: Dr Graham Beards, Wikimedia Commons, CC BY-SA 4.0
Breakthrough is a much overused word but is merited in the context of the recent report that HPV vaccination of teenage girls may reduce the incidence of cervical cancer by around 90%.
This result was widely anticipated but is, nevertheless, a spectacular success. Following on the heels of the SARS-Co-V2 vaccines, this is not only great news for women worldwide but is excellent PR for science and the best possible counter to the anti-vaxxers.
It also sets a striking precedent. Cancer risk prevention to date has derived from prudent avoidance (cigarette smoking and to a lesser extent, solar UVB for melanoma) or most likely serendipity in the case of stomach cancer.
This cancer, which finally toppled Napoleon as well as many in his family, was the number one cancer killer in the 19th century before the era of mass-produced cigarettes but declined in incidence throughout the 20th century possibly due to the widespread use of refrigeration and reduced use of salt as a preservative. Natural decline in Helicobactor infection of the stomach may also have played a part.
Successful prevention
The success of HPV vaccines is the first time a common cancer has been prevented by targeted, science-guided prophylactic intervention. Cervical cancer is the most common female cancer in less developed countries worldwide and a major cause of mortality. As with Covid-19, rolling out protective vaccination against HPV should now be a priority for these countries.
Success did not come easily or quickly. The German virologist Harald Zur Hausen struggled for a very long time to convince his sceptical peers that HPV (principally HPV 16 and 18 variants) did cause cervical cancer. In addition to the basic science, the success of the HPV vaccination programme, initiated in the UK in 2008, as again with Covid, is a logistical triumph.
But it is not yet a perfect outcome. We will not know for another two decades just how protective it is, girls need to be vaccinated before the age of 16 or before they are sexually active, and in the UK, unlike Australia for example, we were slow to recognise the importance of vaccinating boys, the eventual vectors.
The potential benefits of the HPV vaccine go beyond cervical cancer in women as this same virus is implicated in some oral, head and neck and anal cancers in both males and females.
Preventing other cancers
This good news story inevitably raises the question of what other cancers might be preventable in a similar fashion?
If you ask what fraction of cancers are linked, in causation, to infection, the ball park figure usually offered is round 15% (Cancer Research UK quotes 18%). But this is a Western-biased perspective. In the less developed world where 50% of all cancers arise (around 8 million a year), around 40% are thought to have an infectious aetiology, largely driven by HPV, hepatitis virus and EBV.
In addition to these viral cancers, some are associated with bacterial or parasitic organisms (table 1). The mechanisms involved here are not entirely resolved and doubtless mixed including direct cellular transformation with some viruses and a more indirect pro inflammatory impact of bacteria and parasites.
But all these infection-associated cancers are potentially tractable via vaccines. In addition to HPV, both Hepatitis C and EBV have vaccines in trial. A striking but under-recognised fact is that early-stage extra-nodal B cell lymphomas (strongly linked to specific bacterial infections, as with Helicobacter and gastric lymphoma) resolve with antibiotics. For others such as bladder cancer linked to Schistosome parasites, clean water could be the simpler answer.
The potential extent of cancer prevention is therefore considerable. But we may be underestimating the full extent of microbial influence on cancer risk and therefore the prospects for prevention. It is estimated that in around one third of common adult cancers early-stage progression is associated with, and probably driven by, chronic inflammation.
Cancer and the gut microbiome
This is most evident with cancers of the GI tract including oesophageal, pancreatic and colorectal cancers, but may be involved also in a subset of breast and prostate cancers. I have long argued that a similar mechanism applies to the major type of childhood cancer – acute lymphoblastic leukaemia.
The immediate causes of those persistent inflammatory reactions are mostly unknown and probably both varied and complex. But there is a strong suspicion that abnormalities of the gut microbiome are at the heart of the problem. Inflammatory bowel disease (IBD) is a risk factor or precursor lesion for colorectal cancer. IBD has been clearly linked to an underlying deficit in the bacterial diversity of the microbiome and is now undergoing treatment trials to re-boot the microbiome. What impact might this have on incidence of bowel cancer?
Obesity is both very common, indeed an epidemic in the UK and other Westernised societies, and strongly associated with the risk of many common cancers. So much so that Cancer Research UK announced that obesity was as dangerous a cause of cancer as cigarette smoking. I have argued that the assumption of a direct causal link between obesity and cancer could be incorrect.
An alternative is that obesity and some cancers especially of the GI tract are independent co-morbidities that share the same underlying lesion: a deficient gut microbiome. This would be in line with the now well recognised fact that the gut microbiome exerts profound influence on both our metabolism and our immune systems.
If correct this would suggest that tackling obesity via modification of the microbiome might pay incidental dividends for cancer risk.
'Prevention should be our plan A'
HPV vaccination has been a really global initiative, already introduced to more than 100 countries and strongly endorsed by a WHO ambition to eliminate cervical cancer worldwide. This should now encourage us to be more ambitious and optimistic about prospects for cancer prevention.
This in no way negates the urgent need to improve early diagnosis and to develop more efficacious therapy or combination therapeutics that might thwart drug resistance. All these strategies are equally important. But maybe the less glamorous approach of prevention should be our plan A.
| Organism | Cancer subtype | |
|---|---|---|
| Viruses | Human papilloma virus (HPV) | Cervical, oral, head/neck, anal, and some skin cancers |
| Epstein Barr virus (EBV) | Burkitt's lymphoma, Naso-pharyngeal carcinoma, some Hodgkin's lymphomas and leiomyomas | |
| Hepatitis B & C viruses (HBV, HCV) | Liver cancer, some lymphomas (HCV) | |
| Human leukaemia/lymphoma virus (HTLV-1) | Adult T cell leukaemia and lymphoma | |
| Bacteria | Helicobacter pylori | Gastric carcinoma, Gastric lymphoma |
| Salmonella typhi | Gall bladder cancer | |
| Parasites | Schistosoma hematobium* | Bladder cancer |
| Opisthorchis sp.* | Chorangiocarcinoma (Bile duct) |
*Helminth flukes
Table 1: Cancers associated with viruses, bacteria and parasites.