Image: Chemotherapy drip bags
Almost 50 years ago, United States President Richard Nixon declared what has famously come to be known as his ‘war on cancer’. Comparisons were made to an effort that would bear fruit greater than the splitting of the atom or our first landing on the moon.
So, where are we now? Cancer Research UK recently estimated that, currently, half of all cancers, are effectively cured compared to just a quarter 40 years ago. Success? Perhaps. It depends on whether your glass is half full or not.
Magic bullet
What has changed in this time? If you ask enough scientists and oncologists you’ll probably hear the answer ‘targeted therapy’ at least once.
What is targeted therapy? First, consider the origins of a different kind of treatment - chemotherapy.
During world war II, doctors noticed that victims of mustard gas developed deficiencies of their normal blood cells. They questioned whether other (less toxic!) compounds could eliminate cancerous blood cells. Thus, chemotherapy was born. Fast forward fifty years and it has been used to cure patients not just with blood cancers but testicular, ovarian and various childhood cancers too.
So, the birth of chemotherapy followed from the discovery of a substance that affected normal blood cells. Even today, despite its success, we have to choose our chemotherapy doses carefully to minimise effects on normal cells.
On the other hand, targeted treatment Is rationally designed to target something that is only present in cancer cells, and not in normal cells. The idea can be traced back to Paul Erlich, who described a hypothetical Zauberkugel or 'magic bullet' to kill bacteria without harming our normal cells. He essentially described what we now call antibiotics.
More recently this idea was extrapolated to cancers. For example Herceptin, used to treat breast cancer, sticks to a protein that is only over-expressed in cancer cells. It has likely saved thousands of lives across the world.
The soldiers within
If you keep asking scientists and oncologists, it’s likely that you’ll also hear the term immunotherapy.
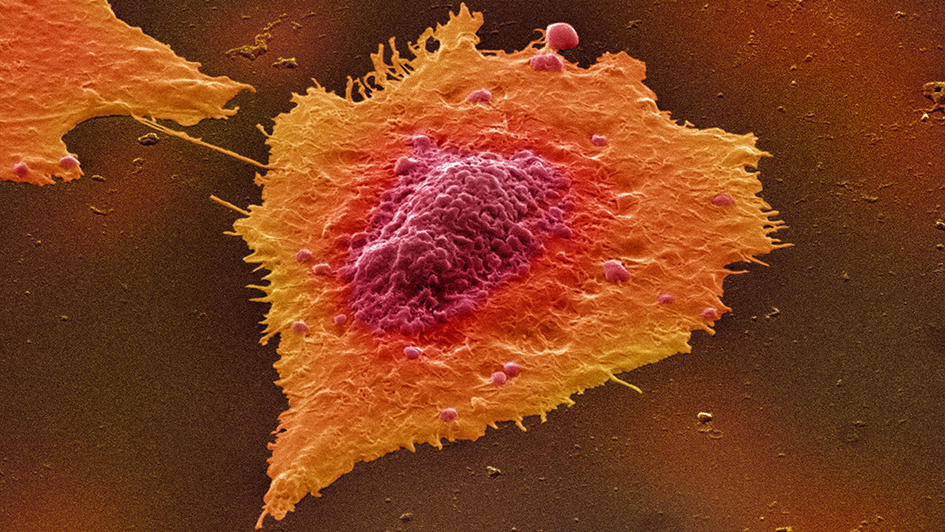
It turns out that we actually have the tools to fight many cancers already; our immune system. This intriguingly complex and elegant system constantly surveys our body for so-called danger signals, like those emitted by bacteria and viruses.
However, it turns out that cancer cells are also dangerous! Therefore, evidence suggests that the immune system keeps a close eye for these dangerous cells and many times destroys them before we even knew they existed.
Unfortunately, sometimes this doesn’t work. Initially, the immune system sticks close to our enemy and keeps the cells in check. Eventually, the cancers trick the immune system into backing off. Like a chameleon blending into its surroundings cancer cells can trick the immune system by changing their appearance.
By blocking this change, ‘immunotherapy’ can make these cancers visible to the immune system again, unleashing its cancer-killing activity. These treatments are revolutionising the treatment of certain cancers such as stage IV melanoma, a disease which was almost universally fatal only a decade ago.
The picture, however, gets more complicated. Not all immune cells are good! Fascinating recent research showed that, after exposure to cigarette smoke, a certain type of immune cell began to help dormant cancer cells to divide and grow bigger.
This is just one tale of an ever-expanding storyline (as well as being another good reason not to smoke)! Watch this space, we are only just finishing the introduction to this immunotherapy saga.
You may have won the battle…
As a clinician scientist, Dr Marco Gerlinger and colleagues noticed that kidney cancers removed at surgery looked very heterogeneous. Each cancer had various colours, textures and patterns within it. Up until this point it was generally thought that a patient’s cancer was a single, uniform, entity.
However, when the researchers used sophisticated molecular techniques to look in more detail they found that actually each patient’s ‘cancer’ was in fact much more than a single entity. Imagine peeling back an orange to find each segment was a different colour.
The implication was huge. Any ‘targeted’ treatment or treatments selected for that patient would have to target all of these so called ‘sub-clones’ to successfully eradicate the cancer. Winning the battle against one clone may be straight forward, but winning the war would require battles on several fronts.
The next chapter
Next year marks the 50th anniversary of Nixon’s declaration. As Tolstoy remarked, “The strongest of all warriors are these two – Time and Patience”, and this story is due to go on for a while longer too. Nonetheless we have made and continue to make great strides.
We are embracing evolutionary biology and learning to detect the segments as soon as they change colour, allowing us to intervene at an earlier stage. Conversely, the best wars are those that were never fought and we are concurrently learning about ways to prevent and detect cancer before the colours appreciably diverge while also improving our techniques in surgery and radiotherapy.
As above, we have begun to learn about the cancer ecosystem. About how the cells interact with immune and other cells around them and how this can affect their regression or growth.
However, while one ecosystem operates within the patient, another operates all around us. As patients, clinicians, academics, industry members and policy makers we must all work together in the interests of our common goal. Only then, will we achieve our mission.
Dr Amit Samani is a Clinical Research Fellow in the Translational Immunotherapy team in the Division of Radiotherapy and Imaging.