Scientists have shed light on how different types of cancer cells in an aggressive childhood brain cancer interact and work together to spread.
Using mathematical modelling, the team provides a framework for detecting, measuring and mapping interactions between different types of cells in diffuse intrinsic pontine glioma (DIPG) – a brain tumour starting in a type of cell known as ‘immature glial progenitor cells’ before spreading to other parts of the brain.
Researchers at The Institute of Cancer Research, London, led the study, published in Cell Reports.
They hope targeting and blocking interactions that allow cells to work together to invade surrounding areas could become a new treatment strategy, which is urgently needed in this currently incurable childhood cancer.
Cells within tumours cooperate
DIPG tumours are made up of more than one subtype of cancer cell. In 2018, the team of scientists at The Institute of Cancer Research (ICR) found the first evidence that different subtypes of cells within a tumour can cooperate – rather than solely compete for resources, as was the common belief.
Their new findings show for the first time that some subtypes have a positive effect on others in terms of how the cells spread – opening up new avenues for testing and developing treatments for this childhood cancer.
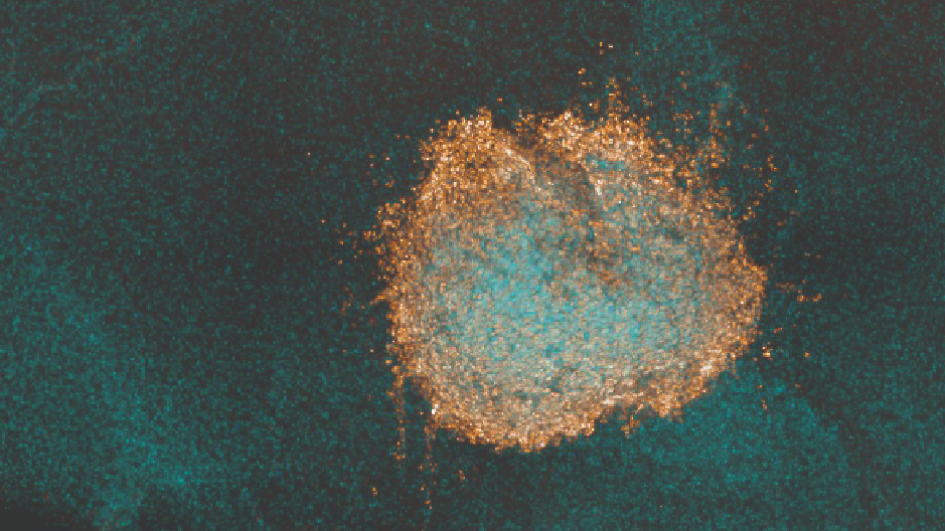
The study, funded by Cancer Research UK, explored the interaction between two different subtypes of cancer cells – labelled VI-E6 and VI-D10 - obtained from donated tissue from patient biopsies, when grown together in the lab. The VI-E6 subtype was able to spread further when grown in a co-culture with VI-D10.
Cooperation more than doubled the spread
Using deep learning to process images from experiments in the lab, scientists were able to identify interactions where one cell subtype cooperated and helped the other grow and spread – and differentiate between these interactions and those where one subtype spread more than the other due to other unrelated factors, such as space restrictions.
Previous models exploring cooperation between cancer cells focused on growth, but this innovative study is the first to measure interactions that affect the way tumour cells spread and invade surrounding areas.
Researchers demonstrated that cells behaved differently when cultured together in the lab, rather than in separate environments. Culturing two different subtypes together more than doubled the spread of the tumour.
When they grew the two different cell subtypes together, researchers found cancer cells were able to spread and invade a greater area. While one subtype travelled and spread more quickly, the speed of the other decreased – highlighting commensal interactions, where one subtype gains benefit without harming or benefitting the other, as well as exploitative interactions, where the fitness of one subtype is enhanced while reducing the fitness of the exploited subtype.
Towards more and better personalised treatment options
The findings demonstrate that interactions between DIPG cell subtypes play a key role in helping tumours invade the local environment and spread – adding to our understanding of how this childhood cancer progresses.
In this way, researchers provide a framework which could be applied to more cancer types. By providing a method of identifying and measuring these cell interactions, the effect of treatments can also be explored.
Researchers are increasingly aware of the importance differences between cancer cells within a single tumour can have on treatment outcomes. Their hope is that identifying and measuring interactions between cancer cell subtypes could lead to better and more personalised treatment options.
The study was co-led by Professor Chris Jones and Professor Andrea Sottoriva, former Team Leader at the Centre for Evolution and Cancer at the ICR.
Attacking tumours by 'disrupting positive interactions'
Study co-leader Professor Chris Jones, Professor of Childhood Brain Tumour Biology at The Institute of Cancer Research, London, said:
“This childhood cancer is incredibly difficult to treat. Nearly all children with DIPG die within two years, and new treatments are urgently needed.
“We are beginning to decipher how different types of cells in DIPG interact and work with each other to fuel the disease.
“By combining deep learning and advanced mathematical modelling with experimental data, we provide a framework for detecting, measuring and mapping these interactions – which we hope will lead to new ways of testing and developing treatments that attack tumours by disrupting positive interactions and promoting negative interactions between cell subtypes.”
'Stopping cancer in its tracks'
Study author Dr Haider Tari, who was part of the Evolutionary Genomics and Modelling Team at The Institute of Cancer Research, London, said:
“If one subtype cooperates with a different subtype in a way that drives the tumour’s growth and spread, it would be crucial to target and block this cooperation – with the goal of stopping cancer in its tracks.
“This innovative study provides a way to identify whether cells are interacting and by how much, and the framework could be applied to a number of different cancer types."
'Discovery research brings hope'
Dr Laura Danielson, Children’s and Young People’s Research Lead at Cancer Research UK, said:
“This study demonstrates the power of mathematical modelling to better understand how cancer cells interact and spread.
“More work needs to be done to understand how we could potentially target these interactions, but discovery research like this brings hope for development of more effective treatments for children and young people affected by cancer.”