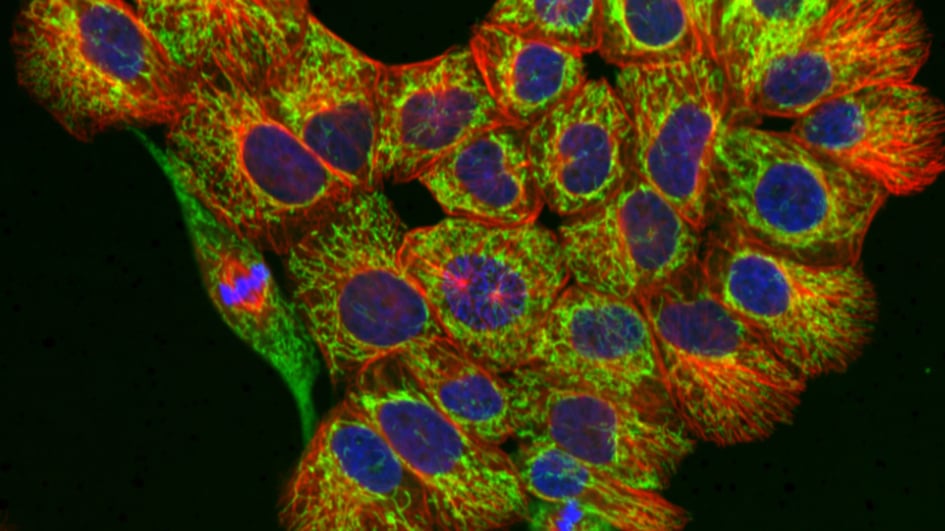
Image: Normal breast epithelial cells with stained mitochondria (green), microtubules (red) and DNA (blue). Credit: Julia Sero.
Researchers have found a way to use a simple, non-invasive scan to tell whether an experimental approach to enhance treatment for breast cancer is effective.
The new research, led by scientists at The Institute of Cancer Research, London, could help doctors visualise tumours and speed up the development of targeted therapies for breast cancer.
The team found that an MRI scan can help assess if experimental drugs targeting and degrading a chemical known as hyaluronic acid are working. By degrading hyaluronic acid, these drugs can enhance the effectiveness of other drugs administered in combination.
The study was published in the journal Molecular Oncology and funded by Cancer Research UK.
A common feature of breast cancer is excessive ‘connective tissue’, which consists of cells and fibres that provide a scaffold upon which the tumour can grow. This dense scaffold is known as the extracellular matrix (ECM) and one of its key components is hyaluronic acid, a chemical that works by absorbing water.
In the context of cancer, hyaluronic acid in the ECM causes tumours to swell, making it hard for drugs to penetrate, reach and destroy cancer cells. For this reason, despite being a well-known and safe skincare ingredient, hyaluronic acid that is naturally present in the tumour’s scaffold is linked to breast cancer spread and poor outcomes when found in tumours’ environment.
Targeting hyaluronic acid
Researchers can use experimental drugs that target and degrade hyaluronic acid to dissolve some of this dense ECM and improve drug delivery to tumours, enhancing their effectiveness.
But when researchers use experimental drugs targeting hyaluronic acid in this way, they often struggle to identify the exact time at which the hyaluronic acid has been degraded, and hence the best time to administer any other drugs.
To address this problem and help guide treatment, researchers performed MRI scans on mice with breast tumours to track the effects of PEGPH20, an experimental drug targeting hyaluronic acid.
They used a scanning approach known as multiparametric MRI, which, as well as providing anatomical images, allows researchers to obtain other measurements that provide additional information about the tissue being analysed. For example, researchers used diffusion-weighted imaging to understand how water molecules moved within tissue.
When they analysed this data, they discovered that a measurement of water’s ability to move or spread, called the apparent diffusion coefficient (ADC), was reduced by up to 38 per cent following administration of PEGPH20. They confirmed that this reduction in ADC was associated with the successful degradation of hyaluronic acid by PEGPH20 through performing additional experiments in the lab.
Improving drug delivery
These changes suggest that PEGPH20 may make breast cancer tissue more accessible to chemotherapy drugs and could potentially improve treatment outcomes.
Using MRI scans in this way means doctors can determine whether drugs like PEGPH20 are working before giving any additional treatment – potentially sparing patients from unnecessary chemotherapy or leading to alternative, more personalised treatment strategies.
PEGPH20 and other similar drugs targeting the dense ECM of breast cancer are experimental and will need to be tested in further clinical trials before entering the clinic.
Disrupting the tumour environment to improve the effectiveness of treatments is a rapidly growing area of interest in cancer research and a key theme within the ICR’s research strategy. Researchers hope their findings could help improve the development of targeted therapies for breast cancer – and potentially other tumours with dense ECMs, such as pancreatic cancer – with the ultimate goal of offering more personalised treatment approaches in future.
Study author Dr Emma Reeves, former Postdoctoral Training Fellow at The Institute of Cancer Research, London, said:
“Our findings could have a significant impact on breast cancer treatment, by providing doctors with a non-invasive and accurate way to assess the effectiveness of drugs seeking to disrupt the tumour’s environment or ‘scaffold’. This could become a valuable tool to deliver more personalised treatments for breast cancer.”
Scan guides treatment
Study leader Professor Simon Robinson, Professor of Magnetic Resonance Imaging of Cancer at The Institute of Cancer Research, London, said:
“Hyaluronic acid helps cells absorb water, which is why it’s such a popular skincare ingredient. But when it comes to cancer, water absorption and swelling in tumours makes it much harder for drugs to penetrate them and destroy cancer cells.
“Experimental drugs like PEGPH20 can break down hyaluronic acid, making it easier for other drugs to reach a tumour by disrupting its dense extracellular matrix.
“Until now, it had proven difficult to find out how well these drugs work in different patients, because they are often given alongside other treatments – so if tumours didn’t respond well to treatment, it was unclear whether that was because PEGPH20 hadn’t worked, or whether the tumour was resistant to the other treatment.
“Diffusion-weighted MRI can be performed on conventional clinical MRI scanners. Our new research shows that we can use such scans to check if drugs like PEGPH20 are working, helping guide treatment in a more targeted and non-invasive way.”